Читать книгу Hemangioma. Questions & Answers - Дмитрий Романов - Страница 4
I. Classification
Оглавление1.1. What classification of vascular abnormalities is common today?
Table 1. Classification of International Society for the Study of Vascular Anomalies
Vascular Tumors
Benign:
· infantile hemangioma;
· congenital hemangioma (RICH, NICH, PICH);
· tufted angioma;
· spindle cell angioma;
· spindle cell angioma;
· pyogenic granuloma;
· other.
· pyogenic granuloma;
· other.
Less aggressive or related tumors:
· Kaposiform hemangioendothelioma;
· retiform hemangioendothelioma;
· papillary intralymphatic angioendothelioma (PILA);
· Dabska tumor;
· complex hemangioendothelioma;
· Kaposi sarcoma;
· other.
Malignant:
· epithelioid hemangioendothelioma;
· angiosarcoma;
· other
* Complex malformations: CVM – capillary-venous malformation; CLM – capillary-lymphatic malformation; LVM – lymphatic-venous malformation; CLVM – capillary-lymphatic-venous malformation; CAVM – capillary-arteriovenous malformation; CLAVM – capillary-lymphatic-arteriovenous malformation.
1.2. Infantile hemangioma and cavernous (capillary) hemangioma are the same thing?
Obsolete terms “cavernous”, “capillary”, “cliff-like” hemangioma, “strawberry congenital mark” etc are used currently. International Society for the Study of Vascular Anomalies (ISSVA) developed classification in 2014 which is recommended for use while determining vascular abnormalities (Table 1). Incorrect terms use makes diagnosis more complicated and confuse communication between doctors. For example, term “capillary hemangioma” might be used for infantile hemangioma, as well as Kaposiform hemangioendothelioma (Table 2).
Table 2. Incorrect terminology used to describe vascular abnormalities.
1.3. What are types of hemangiomas?
Infantile hemangiomas are divided into following types currently:
– superficial (pathological proliferation of blood vessels is determined only on the surface of the skin);
– deep (pathological proliferation of blood vessels is determined in the full-thickness skin and subcutaneous tissue, without skin signs);
– combined (combination of superficial and deep).
Deep infantile hemangioma in the back.
Surface infantile hemangioma in the posterior surface of the lower leg.
Combined infantile hemangioma in the parietal region. Focal form.
Сombined infantile hemangioma in the shoulder area. Focal form.
Also, infantile hemangiomas are divided according to skin lesions range:
– focal;
– multifocal;
– segmental.
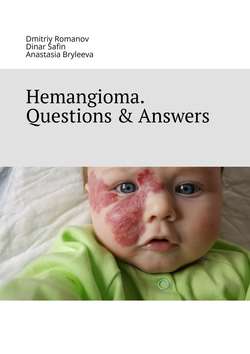
Segmental infantile hemangioma in the right half of the face.
Combined infantile hemangioma in the chest area. The multifocal form.
Segmental infantile hemangioma in the chest and right shoulder.
Congenital hemangiomas are divided into:
– rapidly involuting congenital hemangioma – RICH;
– non-involuting congenital hemangioma – NICH;
– partially involuting congenital hemangioma – PICH.
Rapidly involuting congenital hemangioma – RICH.
Partially involuting congenital hemangioma – PICH.
Non-involuting congenital hemangioma – NICH.
Clinical example. Non-involuting congenital hemangiom.
Non-involuting congenital hemangiom. Newborn.
The same patient. 6 y.o.
1.4. What is the difference between a congenital hemangioma and an infant one?
A congenital hemangioma appears and grows in utero and has its largest size at birth. It does not grow after birth anymore and can decrease and disappear or remain the same size even without treatment.
An infant hemangioma appears basically during first month of baby’s life. In rare cases, a baby is born with it. An active growth of hemangioma begins during first weeks of baby’s life. An active growth phase lasts up to 5—6 months and can last up to 9—12 months. Then, a plateau phase or growth stabilization begins, after that an involution period begins (reverese development of hemangioma) which can take years.
1.5. What is a segmental hemangioma?
If an infant hemangioma affects several anatomical areas at once (e.g., forehead, orbit, cheek and nose on one side of the face or, for example, the wrist and forearm), it is called a segmental hemangioma. In most cases, a segmental hemangioma is located at skin level, e.g. it is superficial.
Why is it so important to separate this nosology? A large damage area can lead to ulceration and bleeding. In addition, segmental infant hemangiomas cab be a signal for certain syndorms presence, such as PHACE (s) and LUMBAR.
Segmental infantile hemangioma in the left half of the face.
Segmental infant hemangioma in the lower half of the trunk and limbs.
1.6. What is hemangiomatosis?
Hemangiomatosis is the appearance of multiple (more than 4—5) small (from 1—2 mm) hemangiomas on the baby’s skin. The number of hemangiomas in hemangiomatosis varies from 5 to 1000 elements on the skin and mucous membranes. Such hemangiomas are located on the surface of the skin, but sometimes there is a combination of small superficial hemangiomas with combined ones.
Hemangiomatosis is of two types:
– benign neonatal hemangiomatosis;
– diffuse neonatal hemangiomatosis. Hemagiomas are present not only on skin but also in liver/spleen/intestines in this form of hemangiomatosis.
Benign neonatal hemangiomatosis. 1000 Infantile hemangiomas.
Benign neonatal hemangiomatosis. Proliferative phase.
Benign neonatal hemangiomatosis. Involutive phase.
1.7. What internal organs can be affected by a hemangioma?
Out of all the internal organs, hemangioma most often affects the liver. Three types of liver damage are distinguished: focal (28%), multiple (57%) and diffuse (15%).
Focal liver hemangioma (28%) is presented by a rapid involuting congenital hemangioma (RICH), which regresses right after birth. The occurrence rate in boys and girls is the same. About 15% of children have infant hemangiomas on their skin. More than 90% of tumor size decreases to the 13th month of life.
Multiple liver hemangioma (57%) is an infant hemangioma, which is often accompanied by skin manifestations (77%). It is usually identified during liver screening in children with hemangiomatosis (four to five or more skin infant hemangiomas). It is 2—3 times more often in girls than in boys. Since all infant hemangiomas develop after birth, multiple liver hemangiomas cannot be diagnosed prenatally. After regression of infant hemangioma, liver parenchyma that is involved in the pathological process (functionally active epithelial cells) becomes normal.
Focal liver hemangioma.
Multiple liver hemangioma.
Diffuse liver hemangioma (15%) is an infant hemangioma which is very often detected during the neonatal period. Diffuse liver hemagioma is not presented by the normal liver tissue, the entire liver is replaced by a tumor. Half of the patients have skin hemangiomas in this case. Girls suffer more often (in 70% of cases).
Diffuse liver hemangioma.
1.8. What is Kaposiform hemangioendothelioma (hemangioendothelioma)?
Kaposiform hemangioendothelioma is a a rare vascular tumor, that is characterized by local aggression, but without metastasis process. The occurrence rate is approximately 1: 100,000 children. It occurs with the same frequency in boys and girls. The head and neck (40%) are more often affected, less often the body (30%) or limbs (30%). It occurs in 60% of cases in the neonatal period and is identified in 93% of cases during infancy. This diagnosis can be made at an older age. Kaposiform hemangioendothelioma can occur in adults.
In 71% of patients with this tumor, life-threatening Kasabakh-Merritt syndrome is identified.
In some cases, differential diagnostic procedure with infantile hemangioma is required.
Kaposiform hemangioendothelioma in the left half of the face and neck.
3d reconstruction of computed tomography with contrast of the patient with Kaposiform hemangioendothelioma.
1.9. What is Kasabakh-Merritt syndrome (phenomenon)?
Kasabakh-Merritt syndrome, also known as hemangioma thrombocytopenia syndrome, is mostly evident by the presence of a large vascular formation (the most common formation is a Kaposiform hemangioendothelioma but there may be others), which is complicated by thrombocytopenia (platelet count reduction), гемолитической hemolytic anemia (red blood cell destruction) as well as coagulopathy (clotting problem). All these factors lead to the severe bleeding. The Kasabach-Merritt syndrome is equally common in boys and girls.
Kasabakh-Merritt syndrome. Kaposiform hemangioendothelioma.
The same patient a general view.
1.10. What is pyogenic granuloma?
The pyogenic granuloma is also called lobular capillary hemangioma. In most cases, acquired granuloma is presented but there are also cases of congenital pyogenic granuloma described. It is basically solid red papule that grows rapidly and usually forms a stalk (pedicle).
Pyogenic granuloma in the area of the nasal slope.
The pyogenic granuloma is characterized by bleeding (64,2%) and ulceration (36,3%) tendency. It can decrease after the bleeding and crust falling off but usually it grows over again. It appears at the age of 6—7 years most commonly but in 12,4% of cases it appears on the first year of life. The pyogenic granuloma mostly affects skin (88,2%), less often the mucous membranes (11,8%). It is found on the head and neck in 62%, body is affected in 20%, upper limbs in 13%, lower limbs in 5% of cases.
Pyogenic granuloma. Bleeding from granulomas.
25% of patients had a history of injury at the pyogenic granuloma location or skin changes (such as a capillary or arteriovenous malformation). The modern theory suggests that pyogenic granuloma inducts secondary reactive skin lesions after injury.
1.11. What else is considered to be vascular tumors?
Angiosarcoma is a tumor characterized by malignancy. It is identified in less than 1% of cases amongst soft tissue sarcomas. Angiosarcoma is extremely rare in children (approximately 1%). It is equally often detected in boys and girls. The average age of diagnosis is 12 months of life.
Cutaneovisceral angiomatosis with thrombocytopenia. This disease is also called multifocal lymphangioendotheliomatosis with thrombocytopenia. Multifocal vascular lesion affects skin and gastrointestinal tract, accompanied by platelet count reduction (thrombocytopenia). Lungs, bones, liver, spleen and muscles are also affected.
Intramuscular Ensinger hemangioma (Ensinger hemangioma is a small vascular type or intramuscular hemangioma – capillary type) is a vascular tumor that occurs in the skeletal muscle. In occurs in children in 25% of cases. The average age of tumor detecting is 25 years.
Epithelioid hemangioendothelioma is a malignant endothelial tumor with an unpredictable clinical course. In occurs in children in 7% of cases. This tumor is usually multifocal and affects skin, bones, liver, lungs (lesion might be bilateral).
Infant myofibroma (term “infant hemangiopericytoma” was used earlier). This is the most common fibroid tumor in infants. There are three forms of infant myofibroma: solitary (common), multifocal (infant myofibromatosis), widespread (internal organs are affected). Up to 60% of cases are detected at birth. The tumor can grow during early childhood. It is detected more often in boys than in girls (1,6:1). It looks like an infant hemangioma very often, which requires differential diagnosis.
Tufted angioma, or Nakagawa angioblastoma. This tumor is clinically and microscopically similar to Kaposiform hemangioendothelioma but it is less aggressive. It can show local invasive growth but does not metastasize. Tufted angioma manifests itself during infancy and early childhood. Just like Kaposiform hemangioendothelioma, tufted angioma can be associated with Kasabach-Merritt syndrome.