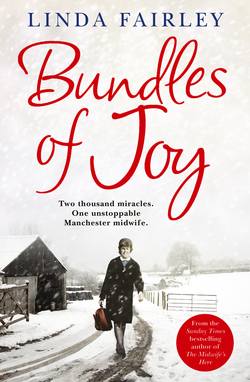
Читать книгу Bundles of Joy: Two Thousand Miracles. One Unstoppable Manchester Midwife - Linda Fairley - Страница 9
ОглавлениеChapter One
‘I’d love to hear some good news’
‘Is there anything I can do to help, Nurse?
Mrs Sheridan’s well-fed son Simon was fast asleep in the plastic cot beside her bed, and she could see that I was run off my feet on the busy new postnatal ward.
‘Actually, yes, that’s very kind of you,’ I replied gratefully. ‘Would you mind wheeling Tina in her pram?’
Baby Tina was a fragile little girl who had been born small for dates and was always hungry, which made her unsettled.
‘It would be my pleasure,’ Mrs Sheridan beamed. ‘Poor little mite, I don’t mind one bit.’
Baby Tina’s mother was a seventeen-year-old girl who had decided to put her daughter up for adoption as soon as she was born. The young mother had discharged herself a few days earlier, leaving Tina in our care until the authorities were able to place her with a foster parent.
All the new mothers on this ward understood the situation, and a few had pitched in over the last day or two to give Tina a cuddle or a ride in her pram, whenever their own babies were sleeping soundly in their cots.
I directed Mrs Sheridan to the nursery, where Tina lay.
‘Call one of the other midwives if Simon wakes up and you need to leave Tina, if she is not settled.’
‘Don’t worry, Nurse,’ she smiled. ‘I can manage, no bother.’
It was Thursday 3 February 1972, and local dignitaries were gathered downstairs, in the entrance to Ashton General Hospital’s Maternity Unit, for the official opening ceremony. I had been told to try to attend the event, and so I slipped away, leaving the staff nurse in charge of the ward.
I quickly took the lift down to the ground floor, hoping to catch a glimpse of the historic moment when Sir John Peel, President of the International Federation of Obstetricians and Gynaecologists, would unveil a plaque on the wall, declaring the unit officially open.
I was a junior sister now and, as I stood at the back of the foyer that day, I allowed myself a moment of reflection and self-congratulation. My husband Graham, proud as ever, had bought me an antique silver buckle to attach to my red belt. I now wore a navy blue dress instead of a pale blue one and I had the ‘frillies’ on the cuffs of my short sleeves.
In becoming a sister in January 1972, one year after qualifying as a staff midwife, I had reached another milestone in my career. I felt a great sense of achievement as I watched the brass plaque being unveiled and listened to a succession of local dignitaries applauding our new 142-bed, £2 million maternity unit.
Sir John spoke of the tremendous advances in obstetrics, and of how modern techniques had combated the once high mortality rate amongst newborns. The Department of Health had achieved its national target of ensuring 70 per cent of births took place in hospital, he said, and in the Manchester Hospital Region the figure exceeded 80 per cent. This meant that our new unit was much needed.
I smiled warmly as a beaming Mrs Randle, the mother of the first baby to be born in the new unit in December 1971, was presented with a silver cup while her son Jarrod slept in her arms, oblivious to his starring role in the proceedings. Lord Wright, Chairman of the Ashton and Hyde Hospital Management Committee, declared triumphantly: ‘We are proud of this unit and we should take pride in seeing the happy, smiling faces of the mothers in the unit!’ The local press turned out to cover the event and, as photographs were taken for posterity, I thought it was a day I would not forget.
Afterwards I returned to the postnatal ward with a real spring in my step. We had this whole five-storey unit all to ourselves, and I loved working in it. Gone were the days when the maternity unit was housed inside the old Ashton General Hospital. We still shared the same grounds, but now our new facility stood alone, a state-of-the-art 1970s steel-framed block, clad with contemporary concrete panels.
I’d excitedly watched the building work progress throughout 1970. I remembered peeping inside as the unit slowly began to take shape, excitedly imagining what it would be like to have ultra-modern plastic cots instead of old-fashioned cloth cribs, shiny store cupboards stocked with luxuries like disposable syringes and razors, and even paper caps and plastic aprons to replace our starched cotton ones. Now, I was actually working here – and as a junior ward sister, no less!
Stepping back inside the ward, I went straight over to Mrs Sheridan, who was rocking a very satisfied-looking Tina tenderly in her arms while her son Simon continued to sleep soundly in his cot. If Lord Wright were to walk in here now, I thought, he’d be delighted to see how well these new wards were working out, and he would indeed see the ‘happy, smiling faces’ he had talked so animatedly about. The atmosphere here was friendly, just as it was on the big open-plan Nightingale wards at the old maternity unit, yet there was a more intimate and peaceful feel to these smaller wards, too, as they were divided into rooms with four beds in each. I liked them very much.
‘Good. You managed to settle her?’ I said to Mrs Sheridan, who was looking very relaxed and had clearly had no trouble with either Tina or Simon.
‘She did ever so well,’ Mrs Sheridan replied, giving me a satisfied smile. ‘Hope you don’t mind, Nurse, but I gave her a little breastfeed.’
‘Pardon?’
‘Well, I knew it would be the only breastmilk she would ever get and I thought it would give her a good start. Simon’s doing so well on my milk that Sister Kelly said she thinks I must be producing Gold Top!’
I gasped, feeling absolutely flabbergasted. Breastfeeding had gone out of fashion at the time, and was nowhere near as common as it is today – in fact, midwives had a job convincing most women of its benefits. The majority of women still asked for a course of Stilboestrol, prescribed to suppress their milk, and most opted to bottle-feed from day one. Mrs Sheridan was clearly not one of those women – far from it!
‘Well, you’ve obviously done a very good job,’ I said tactfully, taking a deep breath and lifting the contented baby girl out of her arms, my brain going into overdrive as I wondered how I was going to handle this one.
At that precise moment some of the dignitaries from the opening ceremony appeared in the corridor outside the ward. Miss Sefton, Head of Midwifery, stood in the doorway and began enthusing loudly about the marvellous new facilities.
‘Most of the accommodation is in four-bedded rooms which combine sociability with quietness,’ I heard her say. ‘And I am very pleased to say that the new unit is attracting the highest calibre of midwives. We are very proud of our staff – in fact Sister Buckley over there is the very midwife you may have seen on the posters advertising the new unit across the region …’
I took a deep breath and smiled over at them. I was normally very proud of the fact I was indeed the midwife who had been chosen to promote the new unit, and had had my photograph plastered all over Ashton and its surrounding area in the previous few months.
At that moment, however, I wanted the ground to swallow me up, and I was willing the entourage not to come any closer.
I can’t describe how relieved I was when the assorted ladies and gentlemen smiled back approvingly and then continued their tour, walking away from me, down the corridor.
‘Well, Mrs Sheridan,’ I whispered, trying hard not to appear as flustered as I felt. ‘Of course it’s not really the done thing to breastfeed another woman’s baby, but I know you have done it with the best of intentions. I shall have to tell Sister Kelly what you’ve done, though, I’m sure you’ll understand.’
‘I don’t mind one bit,’ she replied. ‘Why would I?’
I look back today and am still flabbergasted; not simply by what Mrs Sheridan actually did, but by how much society has changed.
Nowadays, of course, no woman would dream of breastfeeding someone else’s child like that. If she did, it wouldn’t just be a question of informing the senior sister on the ward, who would most certainly not react in the way Sister Kelly did that day, which was to simply roll her eyes and say, ‘I’ll make a note, but there’s no harm done, is there now?’
Blood tests would have to be carried out to make sure the baby had not been infected in any way, and the threat of legal action would be very real, but back then HIV was unheard of, and litigation was a word we rarely heard.
That said, what happened with Mrs Sheridan also reminds me how very little things have changed over the years. Mothers, and the depths of their maternal instincts, have never stopped amazing me, from that day to this.
About a month later, in March 1972, I was working a shift in the antenatal clinic when I saw a name I recognised – Mrs Sully – on my list. My gut reaction was that I was delighted to see this lady was pregnant again. In her case, I imagined those deep maternal instincts must have given her the strength and courage needed to try again, as she had lost her first baby in dreadful circumstances the previous summer.
I would never forget her arriving at the labour ward in the old hospital, brimming with hope and excitement, as she did throughout her pregnancy. I vividly remembered how everything had seemed so normal, until the awful moment I realised her baby’s umbilical cord had prolapsed.
‘There’s something between my legs,’ Mrs Sully had announced, setting off a heart-breaking chain of events. I had ridden beside Mrs Sully on the trolley as we dashed to theatre for an emergency Caesarean. I could see myself struggling to hold the baby’s head back inside her, desperately trying to stop it crushing the escaped cord, which was hanging outside of the poor lady’s body. I recalled seeing Mrs Sully struggling, too. She was thrashing about on the theatre bed instead of falling quickly asleep under the anaesthetic as we needed her to, in order for the surgeon to perform the Caesarean as quickly as possible.
I remembered the absolute chill that went through my body when I realised that Mrs Sully’s baby son was born too late. He survived for just fifteen minutes, having been starved of oxygen in the womb. It was nobody’s fault, just one of those exceptionally cruel twists of fate that occur so rarely, yet prompt you to wonder if there really is a God.
‘I want a hatful of kids, I do,’ Mrs Sully had said to me this time last year, the very first time I had met her in the old antenatal clinic.
I had hoped and prayed that her wish would still come true despite her dreadful loss, and somehow I believed it would.
‘Good morning, Nurse!’ she smiled at me today.
I was delighted to see that the roses Mrs Sully had had in her cheeks when I first met her had returned. She was blooming again, cradling her tiny bump and looking as pleased as punch to be pregnant once more.
‘Good morning, Mrs Sully,’ I grinned back.
I was so relieved that she was still the positive and optimistic person I remembered. There was clearly no need for me to be apprehensive about seeing her again. Some women may have been reluctant – superstitious, even – to see the same midwife, but not Mrs Sully.
‘I’m glad it’s you,’ she sighed, looking quite relieved. ‘I was worried I might have to talk about what happened, go through everything again …’
I gave a little sigh of relief, too. As a midwife, if anything has not gone to plan, it’s always a great comfort to know that the mother understands it was not your fault. Midwives are not miracle workers; we can only ever do our very best in the circumstances, and sometimes, sadly, that is just not good enough. Therefore, I was very glad to see that Mrs Sully was as happy to see me as I was to see her.
I examined Mrs Sully by palpating her abdomen and listening to her baby’s heartbeat with a Pinard’s stethoscope. Everything seemed in perfect order, and I was pleased to note that she was approximately sixteen weeks pregnant and her baby was due in late August. I was absolutely delighted for her; she certainly deserved some good fortune.
‘That day,’ she said wistfully. ‘That day, I could never have imagined ever feeling happy again. Now it seems such a long time ago.’
‘Doesn’t it just,’ I said, and we smiled at each other.
I had turned twenty-four a few days earlier, on 22 March 1972, and I felt more confident and self-assured than ever in my job. Being a ward sister made me walk just that little bit taller. It seemed such a long time ago that I had begun my training as a pupil midwife at Ashton General after three years of nurses’ training at the Manchester Royal Infirmary. In fact it was just two years on, but so much had happened during my time as a midwife.
I remembered wondering, back in 1970, how I was going to manage to deliver forty babies – the required number for me to complete my ten-month training and qualify as a staff midwife. It had seemed such a huge number, but now it seemed so few.
In my first two years I had delivered over a hundred babies, and this new maternity unit seemed to be getting busier by the day as the Government continued to encourage women to have hospital births, believing them to be safer.
‘I don’t know about all this hospital birth business,’ Mrs Tattersall, my community midwife mentor, had said to me on more than one occasion when I was learning the ropes from her as a pupil midwife out in the district.
‘If you ask me, the best tools a midwife has are her hands. They’re the same tools midwives have used since biblical times, and I have always thought you can’t beat them.’
‘Yes, Mrs Tattersall,’ I agreed with her. ‘But then again it’s reassuring to have the paediatricians and doctors, and the theatre on hand if need be, sometimes.’
‘Granted, Linda,’ she said. ‘But a good community midwife should be able to assess when a home birth is not a safe option. Look at it like this. If you give birth at home, there’s a good chance you’ll have two midwives attending – the community midwife and a pupil midwife. What happens in hospital? Tell me that? The place is always bursting at the seams, with one poor midwife trying to look after four or five labouring women all at the same time. Where’s the sense in that? If you’ve got no complications, I can’t see why any woman would choose to be stuck in hospital. That’s a complication in itself, if you ask me.’
I was reminded of this conversation when I bumped into Mrs Tattersall in the car park when I was on my way into work one morning, in the spring of 1972. As usual she had a cigarette in one hand and delivery pack in the other, and she was rushing purposefully towards her trusty green Avenger.
‘What a carry on!’ she complained. ‘What did I tell you about ruddy hospitals?’
‘What’s going on?’ I asked.
‘Flamin’ laundry strike!’ she retorted, charging past me. ‘Can’t stop. Third baby. Waters broke in the Co-op, would you believe.’
As soon as I arrived on the ward I was approached by an agitated Miss Sefton, who was carrying a bag of dirty baby linen. I was startled to see she was wearing a pair of green Wellington boots over her stockings instead of her usual small-heeled court shoes. The boots looked quite comical alongside her immaculately pressed Head of Midwifery uniform, but I tried not to react.
‘Follow me, Sister Buckley!’ she commanded.
Unfortunately, I think I must have gaped at her for a moment, as she chided: ‘Don’t just stand there, follow me!’
I did as I was told, and was amused to see she had turned the bathroom into a makeshift laundry and had been washing baby linen herself, in the bath.
‘Please take over here,’ she said. ‘I have asked the patients to help us out and bring in their own linen and nappies where possible, but we simply cannot have dirty laundry littering the hospital. It is wholly unhygienic.’
‘Right away,’ I said, placing a disposable plastic apron over my uniform before I set to work.
‘Thankfully we have managed to gain access to some twin tubs and dryers that are set up in another part of the hospital, but it’s all hands to the pump I’m afraid,’ Miss Sefton informed me.
The laundry workers’ dispute lasted for about four weeks and the wards became more and more colourful by the day as patients brought in their own bed linen and baby clothes. Despite the newness of the wards, the only colour we were used to seeing was on the pretty floral curtains hanging around each bed. Cot sheets, blankets, bedclothes, nappies and baby nighties were all generally white or a very pale green, chosen to promote a tranquil environment on the ward.
Now, babies were dressed in pale pink, blue and yellow nighties and swaddled in blankets decorated with ducks, trains and goodness knows what else. One little girl even had a frilly lemon-coloured dress on, complete with tiny matching satin bloomers and a mob cap. The mishmash of colours made the wards look quite a muddle, but despite all this, the usual strict routines were adhered to.
For example, each lady was allowed just one or two congratulation cards and a vase of flowers on her locker top. There were never any giant teddy bears or bunches of balloons festooned around the beds as we have today; Miss Sefton would never have allowed such clutter.
‘Come and sit with me and have a hot orange,’ Sister Kelly said to me one morning, when order was finally restored. I can’t remember much about the politics of the laundry workers’ strike, but the workers certainly made the point that they provided a much-needed service which we could not manage without for very long. Trade union bosses secured the promise of improved pay and conditions for the workers, which hastened their return to work.
‘Tell me, Linda, how are yer finding it here on Ward 29?’ Sister Kelly asked.
I watched as she scratched her bosom through her uniform, the same way she had done on the first day I started at Ashton Hospital on 1 January 1970. I smiled to myself, thinking how much I enjoyed working alongside such a familiar character. I was no longer shocked by Sister Kelly’s peculiar habits, and even when she wiped her nose on the back of her hand or wore the same tea-stained dress day after day, I didn’t turn a hair.
‘I absolutely love it,’ I told her truthfully. ‘I’m in my element here, I really am.’
‘That’s good, so it is,’ she said. ‘I’ll let yer in on a secret. I had me doubts about the move, being that much older. But honest to God, I think it’s marvellous here too, I really do.’
She sucked her teeth and looked me up and down.
‘Tell me now, are you and that handsome husband of yours thinking of having babies of your own?’
‘Oh yes, of course,’ I said. I wasn’t in the slightest bit put out by the question. I knew Sister Kelly liked any excuse to have a good chinwag, and this was friendly conversation, nothing more. Twenty-four was a very typical age for a young married woman to be starting a family, and it was something Graham and I were planning for in the very near future.
‘Good for you,’ Sister Kelly replied. ‘I think having a baby yerself can only make yer an even better little midwife.’
I enjoyed talking to Sister Kelly. She was like a mother hen, and she always left me with a warm glow, whatever she said. I wasn’t really sure that becoming a mother myself could make me a better midwife, and Sister Kelly herself was not a mother, but I nodded and enjoyed her friendly and supportive chatter all the same.
A few weeks later, at the beginning of May, I received an unexpected phone call from my father. ‘Linda, your mum has a pain in her back and we’re not going on holiday.’
My dad was always a man of few words, and on that occasion it turned out he excelled himself. The back pain was so severe my mum had been rushed into Ashton General to be checked over, and when I went in to visit her and find out what was going on she told me in a very matter-of-fact manner, ‘I’ve had a heart attack.’
‘What?!’ I gasped. ‘Dad told me you had a bad back.’
Mum looked perfectly fine, and a doctor appeared and explained that the heart attack had been very minor, and that she would be given drugs for angina and allowed home in a few days as long as she promised to rest.
‘Has she been doing too much?’ the doctor asked me.
‘She works hard in our family bakery,’ I explained.
‘Perhaps it’s time she took things a bit easier,’ he suggested. ‘She’s been lucky this time, but this should be treated as a warning to her to slow down.’
‘What a nuisance,’ Mum said. ‘I had my suitcase packed and everything.’ That was typical of my mother. She has a fierce practical streak, and she has never been one to dwell on misfortune.
Mum was kept in for several days, and happily her recovery period was brightened up with the news that she had become a grandmother for the second time, which was a boost for the whole family.
My niece Tijen was born on 15 May 1972 in Vienna, a second child for my brother John and his wife Nevim, and a little sister for my twenty-month-old nephew Kerem. We couldn’t wait to receive a photograph in the post, and when it finally arrived I was thrilled. Tijen looked very sweet, had dark hair and was very petite – a description that still fits her to this day, in fact.
We were all delighted, of course, and I think the new arrival, as well as the shock of suffering the heart attack, made my mother take stock of her life and put a few changes in place. She stopped work in Lawton’s Confectioners, our family bakery, but was never one to sit around twiddling her thumbs, and so she took up pottery and painting. She was very good at both, but it wasn’t enough for Mum. When she was fully recuperated a few months after the heart attack, she asked me if I might be able to find her a little job in the hospital.
‘I can’t just do that, Mum,’ I said initially, not wanting to put myself in an awkward position with my employers.
‘Please, Linda, love. Could you just ask the question?’
That was typical of my mum. She always said ‘if you don’t ask you don’t get’ and, even though I didn’t always feel comfortable sharing that attitude, I admired my mum for practising what she preached. Reluctantly, I phoned the Assistant Matron’s secretary, explained the situation and asked if there might possibly be any vacancies.
‘Actually, yes there are, Sister Buckley,’ came the reply. ‘If your mother can come in for an interview this afternoon we may have just the job for her, but could she start soon?’
Mum couldn’t believe her good fortune and hot-footed it to the hospital a few hours later, whereupon she secured herself a part-time post in the outpatients department of the main hospital, doing clerical work for the ECG patients. She was given a white tunic to wear and told to report for duty the very next morning.
‘Thanks, Linda,’ she said gratefully. ‘It just goes to show …’
‘If you don’t ask you don’t get?’ I laughed. ‘I thought you might say that.’
Still, I couldn’t get over how incredibly lucky she had been with her timing. Something like that could never happen in this day and age. Jobs would never be given out to family members in such a way, and quite rightly so, but this was a different era and my mum certainly benefited from the old-fashioned way of things.
My parents lived in Ashton now and so Mum would even be able to walk to the hospital. Occasionally, we might be able to meet in the canteen for a cup of tea together if our shifts allowed. It seemed meant to be and, all things considered, I felt very blessed with my lot in life.
One afternoon I was sent to work on the antenatal ward as it was short-staffed. I didn’t mind being moved around the wards; in fact I quite liked the change. I usually enjoyed the atmosphere on the antenatal ward. Expectation and excitement always hung in the air, yet there was typically a much calmer vibe than on the labour ward. The women here all had some sort of complication, warranting their stay in hospital before giving birth, which tempered their excitement a little.
It seemed quite peaceful today, despite the ward being full. There was a lady on bed rest who was expecting twins, and several women who were being monitored because they had high blood pressure. One woman, Beryl Johnson, was suffering from a severe chest infection and had been admitted earlier that day for observation and rest. She had the curtain pulled around her bed as she was coughing and spluttering, which made some of the other patients pass remarks.
‘You’d think they’d have put her in a side room,’ one woman said sympathetically.
‘Maybe there isn’t room,’ another replied. ‘Sounds like she’s getting worse, though.’
The women generally didn’t complain, but when they’d been confined to their beds for days or sometimes weeks, they would talk about anything and everything that came into their heads. You might hear them voicing opinions on the latest IRA atrocity or the Vietnam War one minute, swapping recipes or knitting patterns the next or debating whether the Osmonds or the Jackson Five were the best family singing group.
The most popular topic of conversation, of course, was always what had happened to other women they had met on the ward, who had now had their babies and left. At the start of this shift I gathered that a few weeks earlier a patient called Rowena had given birth to a very premature baby, as I heard one of the patients asking my colleague, Susan, how things were with that ‘tiny little mite’.
‘I couldn’t believe my eyes,’ I heard the patient say. ‘What a shock it must have been for Rowena. She was such a lovely girl, too.’
‘What exactly happened?’ I asked Susan when we had a tea break. ‘Oh, Linda, it was quite a drama,’ Susan explained. ‘I’m surprised this hasn’t gone all over the hospital.’
She told me that Rowena had gone into premature labour at just 28 weeks.
‘We were hoping the bed rest might stop things, but she suddenly pushed the baby out, totally without warning! It gave her such a terrible shock. She screamed hysterically, setting the whole ward into quite a panic.’
I dearly hoped the ending of the story was happy for Rowena and her baby, and I listened earnestly as Susan went on to tell me that Stella, a very competent new pupil midwife, was there in a flash.
‘Honestly, you’d have thought she’d been doing this for years. Stella was ace. She wrapped the baby in a towel, tucked it down the front of her uniform and dashed across to Special Care, before you could blink.’
‘And the baby survived?’
‘Yes, he did!’ Susan replied. ‘It was a little boy. We heard he weighed just one pound, eight ounces, but he survived. Rowena has promised to pop in and keep us posted. Fingers crossed he’s doing OK.’
This story inevitably reminded me of Muriel Turner, my patient at the old maternity unit whose premature baby appeared so frail and lifeless I thought he was dead, until he let out a very unexpected but very welcome cry. I relayed Muriel’s story to Susan, explaining that I had carried the baby to the sluice, covered with a towel in a tiny bowl, thinking he hadn’t made it.
‘But he lived too, and he went home after about sixteen weeks,’ I said. ‘Let’s hope Rowena’s little boy proves to be just as much of a fighter.’
Muriel’s story always gave me a good feeling and I never tired of telling it, especially in circumstances like this. In my mind, if Muriel’s miracle baby could survive, there was hope for each and every premature baby, even this incredibly tiny one.
Returning from our break, Susan and I were alarmed to hear that Beryl Johnson’s coughing had intensified quite significantly. Stella was on duty and looked extremely anxious as she stepped out through the curtain pulled around Mrs Johnson’s bed.
‘I’ve tried to make her as comfortable as possible,’ Stella said. ‘She’s sitting in a chair and I’ve encouraged her to sip some water, but nothing seems to be working.’
It was at times like this that I was grateful for my nurses’ training. Sometimes pregnant women are actually ill rather than suffering from a complication related to their condition, and I thought that perhaps an antenatal ward was not the best place for Mrs Johnson. She was thirty-six weeks pregnant, and the strain of coughing so vigorously must have been absolutely exhausting for her. She had been treated by her GP for repeated chest infections, but clearly none of the medication she had been given had managed to ease her chest or get the infection under control.
I offered to take over from Stella and found Mrs Johnson propped up uncomfortably in the chair, clutching her abdomen protectively each time her body choked out another wheezy, involuntary cough.
‘I’m going to move you into a side ward and call the medical registrar,’ I told her.
‘Thank, huurgh huurrrgh th-thank you,’ she spluttered.
The effort of speaking seemed tremendous. Mrs Johnson had bags under her eyes and not just dark circles but nearly black ones, and deep lines creased into her forehead. I saw from her notes she had recently turned thirty-five, but she looked ten years older. Her breathing was so laboured in-between coughs that she sounded like a person with severe asthma, and it was very apparent she needed more than the antenatal care we could give her on this ward.
Transferring her into a vacant side room along the corridor was difficult. Evelyn, a strong and capable auxiliary, helped me to guide Mrs Johnson into a wheelchair, but by now she was coughing so violently I was willing the medical registrar to arrive any second to take over the care of this patient.
‘The doctor won’t be long,’ I reassured Mrs Johnson as I pushed the wheelchair as close to the window as possible, which Stella quickly opened.
‘Don’t try to talk, just concentrate on your breathing, help is on its way.’
She nodded gratefully but she had a frightened expression on her face every time she fought for breath, and she looked absolutely worn out. ‘I’ll leave her in the wheelchair for a minute or two before trying to move her,’ I thought. I sincerely hoped her coughing wouldn’t trigger contractions, as her lungs were in no fit state right now to support her through labour.
Suddenly Mrs Johnson’s eyes flashed and rolled in her head.
‘Th – ha – h – hurgh. Hurgh HURGHHHH’ she spluttered, throwing her right hand up to her chest and slumping dramatically forward in the wheelchair.
My own heart tightened. I could scarcely believe it, but I knew exactly what was happening. Mine and Stella’s startled eyes met temporarily. We both knew what to do and, drawing strength from a fear-loaded adrenaline surge, we manoeuvred Mrs Johnson onto the floor as quickly and carefully as possible. I started working on her chest and instructed Evelyn, the auxiliary, to run for help.
‘Unless you ladder your stockings, to my mind you haven’t made a good job of dealing with a cardiac arrest!’ I could hear Sister Hyde’s voice in my ear. That’s what my old mentor had taught me on my very first day under her wing on the cardiac ward at the Manchester Royal Infirmary, and right here, right now, I was putting that training into practice with all my might.
Stella and I worked desperately on Mrs Johnson, giving her cardiac massage and mouth-to-mouth resuscitation. The medical registrar had arrived in the side room within moments, and he worked with us, offering words of encouragement as he did so. Stella had taken the same route as me into midwifery and was a newly qualified State Registered Nurse (SRN), and we worked well together.
My heart was pounding ten to the dozen as I worked on Mrs Johnson, but that did not stop my brain focusing on the job in hand and doing everything in my power to try to save my patient’s life.
The crash team who deal with patients who have had a cardiac arrest arrived and took over the resuscitation. They began pushing down on Mrs Johnson’s chest, trying to keep her heart beating, but the awful truth was starting to dawn.
Nothing seemed to be making any difference. It was one of those absolutely tragic situations where you are following all the correct procedures, doing the very best you can, but it is simply not enough. Mrs Johnson had had such a massive heart attack her life was possibly already lost before we started our desperate attempts to resuscitate her.
It wasn’t until the moment when Stella and I looked across at the registrar, who gave the signal for everyone to stop trying to resuscitate Mrs Johnson and move away from the patient, that the enormity of what had happened began to hit me. This lady had died right in front of me, and her baby’s life was lost, too. It was so horrendous the shock came over me in wave after wave.
I felt battered and wrung out. I tried to imagine Sister Hyde had been watching me, and that now she was reassuring me that I had done my very best, despite the unthinkable outcome.
I can’t remember walking into the kitchen, but I know I sat very quietly alone in there with my thoughts for some time, drinking sweet tea. I felt the gentle hands of colleagues rubbing my back, and soft words being whispered around me. Nothing soothed my pain, however. I ached all over, and deep within my heart.
At around 5.30 p.m. Mr Johnson arrived at the hospital to see his wife. He had been ushered to sit in a side room by a rather nervous and unprepared female doctor called Dr Bodsworth, and I was called in, too. I looked at my watch and registered it was about half an hour since Mrs Johnson’s death, though if someone had told me I had been sitting down in the kitchen for three minutes or three days I would have believed them. I absolutely dreaded seeing Mr Johnson and I had to peel my eyes off the ground to look at him as I entered the side room.
He was looking worried but not panic-stricken, and we greeted each other with a polite ‘Hello.’ Mr Johnson had clearly come straight from work. He was wearing a mechanic’s boiler suit and still had traces of oil on his hands, though he smelled strongly of Swarfega, a heavy-duty cleaner he must have used hastily on his skin when he got the message to come to the hospital. I recognised the distinctive smell because Graham used it sometimes when he tinkered with his car.
‘I’m sorry, but I have to tell you your wife has arrested,’ Dr Bodsworth told Mr Johnson plainly.
‘I see,’ Mr Johnson said, nodding his head sagely but looking rather bemused. ‘She’ll be all right, though?’
‘No, Mr Johnson, your wife has arrested,’ Dr Bodsworth repeated, more slowly this time.
He looked to me, clearly not understanding the terminology.
‘I’m very sorry, Mr Johnson, but your wife has died,’ I said quietly.
The words seemed to hit him like a bullet in the stomach. His head dropped and he crumpled over in his seat and stared at the floor.
‘The baby?’ he asked eventually, looking up at me pitifully.
‘The baby’s died, too. I am so sorry.’
The three of us sat silently for what felt like an age until Mr Johnson asked, ‘Can I see her?’
‘Yes, of course,’ I replied, glancing at Dr Bodsworth for approval. ‘Come with me. She is in Room 2.’
Dr Bodsworth did not stop me, but she looked agitated. I had heard that she had questioned why no attempt had been made to deliver the baby, but I knew this was an inappropriate question to have asked, and nobody deigned to answer it. In the circumstances we had to try to save the mother first. That was correct medical procedure. We might have got Mrs Johnson’s heart going and been able to perform an emergency Caesarean in the operating theatre, but it hadn’t happened like that. We weren’t to know what the outcome would be and we did what was required, swiftly and efficiently. Nobody was at fault. Nothing more could have been done, but nothing we had done had been enough.
‘I’m very sorry about the baby,’ I said to Mr Johnson, my voice cracking as we each took a seat beside his wife.
Mrs Johnson just looked as if she was sleeping, with the blanket pulled up over her chest and her arms flopped casually over the top of it. Mr Johnson squeezed his wife’s left hand, smudging it with oil from his own hand.
‘I wouldn’t have wanted the baby without … my Beryl,’ he whispered, staring at the wedding band on her finger.
Noticing the oil mark he’d made on his wife’s skin, Mr Johnson looked at her face and said apologetically, ‘Sorry, love,’ just as if she could hear him. I gulped and tried to stop the tears that were welling in my eyes from splashing down my cheeks, but I failed.
Mr Johnson tried to rub away the black mark from his wife’s pale skin, but made it worse. ‘What a mess,’ he gasped, letting go of her and holding his head in his hands as he broke down. ‘What a bloody mess.’
All these years on I still find it very difficult to revisit that day’s events. I thought long and hard about whether to include Mrs Johnson’s death in this book, but it did happen and so I decided I should. Her death was unusual in the extreme, however, and I certainly do not want to frighten anybody, particularly any pregnant women.
We found out from the post-mortem some weeks later that Mrs Johnson suffered from an extremely rare syndrome that affects blood pressure and heart rate and had unfortunately never been diagnosed. Her repeated chest infections most probably exacerbated her condition, but ultimately it was the little-known syndrome that killed her.
Even before the post-mortem results came back with that information I was sure in my own mind that Mrs Johnson’s death was unrelated to her pregnancy. I desperately wanted to reassure the other women on the antenatal ward, who inevitably knew about the tragedy, and I chose my words carefully.
‘Please don’t worry yourself unnecessarily,’ I told each and every one of them as the terrible news began to spread, setting off a very upsetting chorus of gasps and sobs. ‘We do not know the exact cause of her death, but we do know that Mrs Johnson was not a well lady.’
I knew the women were all dreadfully sorry to hear the news, but a survival instinct kicks in with a pregnant woman, and the number-one priority is always her own baby, which she will protect at all costs. What these ladies desperately needed to know was that what killed Mrs Johnson was not going to strike them and their unborn child down, too. Even before the official cause of death was confirmed, I knew my message had to be that they and their baby were as safe as they were before Mrs Johnson ever arrived on the ward, which was the truth. It was right that they focused on that positive and didn’t dwell on negative thoughts, because the alternative was unthinkable.
‘So it wasn’t the pregnancy that killed her?’ several of the ladies asked me, one way or another.
‘No, I believe not,’ I replied. I smiled reassuringly at each pregnant lady and tried my hardest to put on a brave face, but inside I felt cold and sick.
‘Thank goodness for that,’ came the reply over and over again. ‘What a terrible thing to have happened.’
At the end of my shift I sat in the kitchen alone, gathering my thoughts. Losing Mrs Johnson reminded me of other deaths I had encountered at the MRI, which I had found very difficult to cope with. Avoiding death is what led me into a career as a midwife. I wanted to bring new life into the world, not deal with illness and death, and now look what had happened. How could this have happened to Mrs Johnson and her baby?
‘Linda, have you heard?’ Stella said, breaking my thoughts.
I looked at her blankly.
‘Have you heard about Rowena’s baby?’ she added. ‘I thought you might like to hear some good news.’
I had to think for a moment before realising Stella was talking about the tiny premature baby she had carried to Special Care down the front of her uniform.
‘I’d love to hear some good news,’ I replied.
‘He has gained two ounces already and is doing remarkably well. The milk bank’s done him proud. Isn’t that great?’
‘It is,’ I replied. ‘It really is! Do the ladies on the ward know?’
She shook her head. ‘Not yet.’
‘Well, I think you should go and spread the news,’ I smiled.
The milk bank was a stock of breastmilk collected from women on the wards who had a surplus after feeding their own baby. We got them to pump it into glass bottles so it could be used to feed the babies on Special Care, and it was always good to be able to tell other mums their milk was working its magic and helping another baby. The fact Rowena’s fragile little boy was doing well was extremely uplifting, and just the news the whole ward needed.
Stella and I shared a look that told me she was thinking exactly the same thoughts as me. It’s an emotional rollercoaster, working as a midwife. You just never know when you might be plunged into a dark abyss, or when you may be launched back up into the bright sky. As I prepared to leave for the day it was very heartening to hear a succession of ‘oohs’ and ‘aaahs’ filling the ward as news of Rowena’s baby travelled fast.
I thought that Stella seemed to have coped with Mrs Johnson’s death well, perhaps better than I had. She had dried her eyes quickly and got on with the job in hand, looking after the other patients on the antenatal ward efficiently yet compassionately.
I wondered if it was because she had finished her nurses’ training so very recently, whereas I was far less used to dealing with death nowadays. Thank God I had become a midwife, I thought. Thank God that tomorrow I would be back on the postnatal ward, where I would have the honour and joy of helping to care for a brand new life.