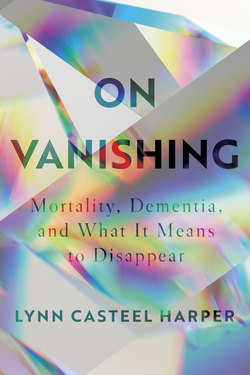
Читать книгу On Vanishing - Lynn Casteel Harper - Страница 8
На сайте Литреса книга снята с продажи.
Оглавление1
Introduction
WITH VANISHING ON MY MIND, I CROSSED CENTRAL Park to the Metropolitan Museum of Art on a late autumn morning on a sober errand. Ginkgo leaves, freshly fallen, coated my path. My root-word research on “vanishing”—which, like “vanity,” comes from the Latin evanescere (“die away”) and vanus (“empty void”)—had led me to a genre of still-life painting that flourished in the Netherlands in the early seventeenth century.
The vanitas school of painting takes its name from the Latin version of an Ecclesiastes refrain (“Vanity of vanities! All is vanity”) and it involves carefully juxtaposing objects deemed symbolic of life’s brevity and the evanescence of earthly achievements. Objects such as mirrors, broken or tipped glassware, books, decaying flowers, and skulls are meant to encourage viewers to contemplate their own mortality. Jacques de Gheyn’s Vanitas Still Life, the earliest known vanitas painting, hangs in one of the Met’s seemingly less popular galleries. Most visitors pass through this corridor of dark still-life paintings on their way to lighter, more moving pieces. That autumn morning, I had Vanitas Still Life to myself.
A modest-sized piece, 32.5 by 24.25 inches, it contains a panoply of vanitas symbols. A thin stream of vapor rises from an urn, an orange flower with browning leaves languishes in another. Dutch medals and Spanish coins glitter in the foreground. Two philosophers—Democritus, the “laughing” philosopher, and Heraclitus, the “crying” philosopher—recline in the painting’s top corners, pointing to the objects below. A large transparent bubble hovers above a human skull. From every angle, the viewer confronts images of life’s transience, but it is the skull that serves as the central reminder of human vanishing. The empty eye sockets locked my gaze, making me think—vainly—of my own future. A hollowed head, more than any other bodily remnant, symbolizes death’s totality, an unyielding force that consumes the entire person, even the ability to think. I guess there’s a reason why the sight of Yorick’s skull, not his rib cage or pelvic bone, occasions Hamlet’s famous lament.
As a condition associated with the head, dementia—like the vanitas skull—ignites an especially acute awareness of mortality, placing our very selves under death’s scrutiny. In the last decade, I have glimpsed dementia from several different angles. I have seen dementia-related deaths in my own family. I have worked with dementia sufferers day-to-day in my capacity as a nursing home chaplain. I recently discovered that both of my parents carry one copy of ApoE4, a gene variant strongly linked to late-onset Alzheimer’s disease. I have a 50 percent chance of having a single copy of the gene, which doubles or triples my risk of developing the disease. I have a 25 percent chance of having two copies, which elevates my risk by eight to twelve times, giving me a 51 to 68 percent chance of having Alzheimer’s by the time I am eighty-five. My particular bloodlines aside, the chance of getting Alzheimer’s disease, the most common form of dementia, is one in nine after age sixty-five and one in three after eighty-five. Nearly six million people in the United States are living with Alzheimer’s—making it the nation’s sixth leading cause of death. And yet nuanced thinking about dementia is largely absent—perhaps even nonexistent—in public discourse.
Heart disease impairs circulation. Kidney disease impairs filtration. But brain disease impairs communication. By distinctly and directly impacting our abilities to relate with ourselves and others, it confronts us with the fact of our humanness: to be human is to be limited, even in our most cherished capacities. Perhaps more than other conditions, dementia brings our fundamental lack of ultimate control over our lives, and their endings, to a head.
Rather than confirming the humanness of sufferers, dementia, curiously, is often viewed as throwing it into question. A gerontologist once told me over lunch that he begins his dementia caregiver workshops by telling participants that their loved ones remain persons throughout their illness. He reminds caregivers that, even as their relatives become more inaccessible, their “core” never leaves. I am glad for his admonition; I am also troubled that it is needed. I doubt caregivers of persons with terminal heart disease need such instruction, or caregivers of infants need reminders that, even though their babies cannot talk or use the bathroom, they remain people.
That we need reminders that persons living with dementia are “still people” elevates my curiosity and my suspicion about the peculiar burdens dementia-causing diseases bear. We seem to have placed dementia beyond the scope of ordinary human imagining, as if this condition alone reveals some nasty, shameful secret: the ease with which we all may disappear.
The cultural critic Susan Sontag’s classic Illness as Metaphor emerged from her rage at seeing, after her own cancer diagnosis, “how much the very reputation of this illness added to the suffering of those who have it.” In 1978, Sontag contended with cancer’s reputation as scourge, invader, predator, demonic pregnancy, demonic enemy, barbarian within. Cancer’s roots were then imagined, at least in part, as psychological, resulting from repressed emotion. These metaphoric conceptions of cancer saddled its sufferers with shame and prevented many from seeking proper treatment or even knowing their diagnosis. A decade later, in AIDS and Its Metaphors, Sontag turned her critique to popular metaphors surrounding AIDS, the new “scourge,” which gravitated toward the language of contagion and contamination, carrying an even greater charge of stigmatization. AIDS, Sontag wrote, was among “grave illnesses regarded as more than just illnesses.” It was perceived “not just as lethal but as dehumanizing”; it supposedly degraded and dissolved the person. Sontag hoped that even this disease, so “fraught with meaning,” could become, one day, “just an illness.”
In our contemporary moment, I think Alzheimer’s has become another disease “fraught with meaning.” It, too, is regularly spoken of as a force that degrades and dissolves a person. Rather than the fear of invasion or contagion, it evokes the fear of advancing oblivion. The disease is “the long goodbye,” people say, or “the death that leaves the body behind.” The afflicted become the “living dead,” who have vanished in plain sight. We are taught to think that dementia displaces persons, turning their faces to “blank stares” and their bodies to “shells,” making strangers of intimates. A thief, kidnapper, slow-motion murderer, Alzheimer’s purportedly robs, steals, and erases one’s memory, mind, personality—even one’s very self. That persons with dementia are so readily envisioned as vanished or vanishing, succumbing to an especially terrifying, slow-moving, unstoppable vortex of suffering, surely speaks to anxieties beyond the ordinary fears of death and disease. The intense negativity of dementia metaphors—combined with their ubiquity—moves them beyond vivid description of brain disease; they express an outsized dread. It seems dementia has become more than just an illness.
I worry that the language we think describes a reality also creates one, that Alzheimer’s notorious reputation adds to the suffering of those who have it, their caregivers, and everyone else in the at-risk population—that is, all of us who plan to grow old. Images of vacancy seem to push persons who do not have dementia away from those who do, keeping “us” at arm’s length from “them.” If “the light’s on but nobody’s home,” why would I (or anyone else) wish to visit?
The story of how I became involved with dementia is not entirely straightforward—perhaps mirroring the oblique course of dementia itself. I can trace some of my interest back to the summer after I began divinity school, the summer I turned twenty-four, when I completed my first unit of chaplaincy training in a hospital. I was reluctant to enroll in the ten-week program, fearing I did not have the constitution for this kind of work. The last time I had been inside a hospital was five years prior, when I had visited a friend who had been in a motorcycle accident. When she described the pins screwed into her hips, I fainted and fell backward, hitting my head on the cold ceramic floor. I spent the afternoon in the emergency room for observation.
But with no other prospects for the summer, I applied to the program, and was assigned to a neurological unit where patients were recovering from brain surgery. They had had tumors, aneurysms, strokes. I spent each day with patients who struggled to find words, to relearn basic tasks, and to just stay awake. I learned about brain death when I was called to the room of a teenage kid who had crashed his four-wheeler into a tree. His mother’s knees buckled when she received the news that her son was brain-dead.
The fragility of the brain pressed in upon me, and I began to confront how closely I had tied my sense of identity and worth to my own intellectual ability, a metric that now felt remarkably tenuous. I wanted to push away this disquieting insight, but grappling with the brain’s changeability would not leave me so easily. Two weeks after I left the hospital, I began a requisite yearlong internship. My placement was a continuing care retirement community, also known as a CCRC, which, I learned, is a campus that contains tiered levels of care, including independent living, assisted living, and skilled nursing or “nursing home” care. Rather than the acute brain traumas I encountered in the hospital, this assignment exposed me to the ordinary frailties of aging minds.
I shadowed the community’s two chaplains—Maurice and Ray. I recall Maurice listening with great attention to a woman with severe dementia. While I could not make any sense of what she was saying, Maurice seemed utterly engaged. Later, he spoke to me about the importance of listening to patients’ word fragments and connecting them to Latin morphemes. At the time, I found this lesson a bit tedious and far-fetched, but what strikes me now is how seriously he had taken her, how he had presumed a meaningful interaction was possible. The woman was not lost to all meaning—she needed careful and creative interlocutors and interpreters.
Each week I accompanied Ray to the Memory Enhanced Residence, a small wing of the facility where a dozen or so residents who had dementia lived in a homey environment, with a shared living room and dining table. After Ray read from the Bible and gave a brief reflection, he would ask a resident named Thelma to give the closing prayer. She had been a pastor’s wife, and the intonation and fervor of her prayers reflected decades of blessing meals, church meetings, and Sunday school classes. While I did not always follow the logic of her prayers, how one sentiment connected to the next, I sensed their sincerity and the calm assurance that overtook Thelma and that touched me, too.
After I completed my Master of Divinity degree, I began a nine-month chaplain residency program at a New Jersey hospital. One of my three assigned units was in the basement next to the morgue. It was designated for patients who had chronic conditions such as emphysema, who were not acute enough for the ICU but not stable enough to go home. Most of these patients were old. As the year progressed, the unit began to house mentally ill patients who had come to the emergency room and were waiting to be transferred to a psychiatric hospital. Physically frail old people and psychologically fragile adults of all ages were lumped together in the bleak, remote bowels of the hospital—a sad picture of the wider culture’s exclusion of these same populations. Perhaps this combination of patients was preparing me to understand some of the stigma around older persons with dementia. I spent a disproportionate amount of my time on this unit, finding many of its occupants starved for human encounter beyond what was clinically expedient or cognitively normative. Regular back-and-forth conversation held little comfort for many of these patients, who did not have the energy or attention for words.
A few months after I completed the residency, I was hired as the chaplain at a 1,400-resident CCRC on the New Jersey Shore. The campus contained eight buildings of independent living apartments, connected by hallways and a sky bridge, and one five-story building of assisted living and skilled nursing rooms. I served the residents who lived in this latter facility, called the Gardens, which sat on the edge of campus, detached from the rest of community. It was here where my specific passion for persons with dementia and for the philosophical and spiritual issues surrounding the mind’s vulnerability was forged.
On my first day at the Gardens—the first day of nearly seven years—an administrator gave me a tour of each of the five floors. The only part of the tour I recall is my introduction to the fourth floor, a skilled nursing unit that had been designated for residents with severe dementia. I have a hazy memory of stepping just inside the doorway of the unit’s large activity room. A young staff member, wearing a Hawaiian shirt and floppy straw hat, supported an old man by the elbow as he lumbered across the room. I do not recall with clarity any other individuals who filled the room that day, only wheelchairs and slumped bodies. My guide told me that I would likely not spend much time here. With nearly two hundred residents under my care, I would find other (better, more productive) ways to fill my day than visiting persons who would forget me the moment I left.
Memory is tricky. I now wonder if he had indeed expressed his prejudices to me directly, or if I absorbed them indirectly, or if I simply carried them within myself. Nevertheless, I received a clear message, consistent with a dementia-phobic culture: my presence would not be needed with these particular residents, my absence would not be noticed. The unspoken corollary: I would not need these persons’ presence or be impacted by their absence. They were considered to have disappeared from themselves, and I was expected to disappear from them.
In 2014, I left the Gardens and moved to South Carolina, where my husband had accepted a two-year visiting academic appointment. During this period, I feverishly read and wrote about dementia and spirituality. I also began facilitating occasional workshops on the subject, as faith groups asked me for help in relating to their congregants with dementia. Populated mostly by professional and family caregivers, these workshops have kept me in direct dialogue with people who are intimately invested in the lives of persons who have dementia. After my husband’s position ended in 2016, we moved to New York City, where I became the minister of older adults at the Riverside Church, a large interracial, interdenominational congregation in Upper Manhattan. Working with elders at the church, as well as leading workshops, continues to connect me to issues surrounding brain aging. But it was my time at the Gardens, which overlapped with the last years of my grandfather’s life with dementia, that served as the crucible in which this book was formed.
The closer I came to people with dementia, the more my assumptions vanished, the more they became individuals rather than a blur of disability. While I encountered diminishment and loss on the Gardens’ dementia unit, there was more than just deterioration. At times I felt I was witnessing, instead, a kind of ascendency—of compassion, honesty, humility. I befriended Evelyn, a retired math teacher, who spoke to me as a colleague, often asking, “How are your students?” I met Mary, who, despite her acute anxiety, readily assisted her less-mobile neighbors, pushing them in their wheelchairs to activities and meals—and who once helped me plan a party. I met Bernice, who taught me that not all of the disappearances associated with dementia prove unwelcome or tragic. What vanished in Bernice’s later years were some of the distressing manifestations of her long-standing mental illness. Crippling anxiety and paranoid delusions gave way to more laughter and delight. One day she pointed out my gray hair, grinned, and declared, “See, you’re aging, too! Just like us!”
I came to know these residents and so many more—not primarily as defective victims of Alzheimer’s, presumed to be “lost” to their disease—but as complex, dynamic individuals. And I began to wonder: why do we—those whom the dementia activist Morris Friedell termed the “temporarily able-brained”—need them to vanish? Why are we so eager to view them as disappearing or disappeared? And what possibilities are we precluding, what hard work of the soul are we avoiding, by imposing this distance?
I want to probe the distance. I want to understand why certain metaphors dominate, eclipsing other ways of imagining dementia, and how these depictions of dementia generate and reinforce stigma. I want to interrogate the cultural, social, political, and spiritual values that disproportionately define us by certain cognitive capacities. I am searching for new, more robust renderings of dementia that expand our vision beyond progressive vacancy and dread.
It was Betty who originally stretched my imagination. In my first months at the Gardens, Betty helped initiate me to the fourth floor’s rich potential. She always carried a floppy, well-worn Bible on her lap, as she wheeled herself up and down the unit’s hallways. When I suggested to Betty that she and I start a Bible study on the floor, she happily agreed. On Thursday afternoons, with a few of her neighbors, we began to gather in a small dining room across from the common room. I had no idea what to do, so I began at the beginning, reading stories from Genesis. Betty, who kept her eyes closed most of the time, came forth with great insights and funny quips, but only after she had sat in silence for many minutes. On the afternoon I read the story of Joseph’s brothers throwing him in a pit and selling him into slavery, she exclaimed, “Oh, the jealousy!” as the other participants were dispersing after our closing prayer. I learned that her long silences did not mean she was disengaged. She taught me to slow down and wait with my mouth shut.
Like any good evangelical, Betty lamented that the group was not bigger; she wanted converts, new recruits. She had imagined throngs, not just three or four acquaintances in a small circle. Her passion for engaging others struck me as utterly loving, a thoroughly intact desire to reach beyond herself. Betty’s tireless energy laid the groundwork for the group to flourish after her death. Although perhaps not quite in the way she would have hoped, the group did grow, evolving into an interfaith spirituality group of nine or ten devoted attendees. Our meetings became the highlight of my week. Whether facilitating this group, visiting with residents and their families, or chatting with stretched-thin staff, I found I spent more time on this floor than any other.
The Buddhist nun Pema Chödrön says we work on ourselves in order to help others, and we help others in order to work on ourselves. We go into the areas of society that we have rejected so we can reconnect with the parts of ourselves we have rejected. I spent time on the dementia unit not because I was some kind of martyr or saint, or because the work came preternaturally easily to me (it did not), but because, perhaps, I sensed I could mature as a minister—as a person—only if I learned how to embrace those people whom we can all too easily believe have nothing to offer. Perhaps, in the process of knowing them, I might come to embrace the seemingly unworthy—confused, strange, fragmented—parts of myself. If my faith was supposed to culminate in cheerful bedside conversations, erudite sermons, eloquent prayers, unending activities and activism, and word-heavy worship services, then I (and the larger tradition of which I am a part, as a Baptist minister in the mainline Protestant vein) would have little or nothing to learn from persons with dementia, and even less to offer them. But I began to see my faith—and my role—in different terms. I think dementia—the process of turning it over in my mind, investigating it, and above all, coming close to persons living with it—has slowly stretched my imagination about spirituality, asking me to value silence and absence, to embrace strangeness and spontaneity, to revere the nonverbal and nonlinear.
Around the time I began working at the Gardens, my own family was encountering up-close the depths of dementia. On the morning of my grandparents’ weekly shopping trip, the teenage boy whom my mother had hired to shuttle her parents around town found my grandfather on the lawn mower and my grandmother unresponsive in bed. Apparently, unable to rouse his wife of sixty-five years, my grandfather had gone outside to mow the lawn.
My grandmother’s sudden death exposed the hundreds of ways she had compensated and covered for my grandfather’s dementia. What we had dismissed as hearing loss, a bout of depression, or a touch of senility, revealed itself as something progressive and pervasive. Overnight, my mother became his caregiver. My mother and her father were living in an intimate way what I was encountering in a professional setting half a country away. Unlike me, they did not leave the dementia floor at five every evening; they were grounded in the round-the-clock realities.
During the year I began writing this book, and just a few months after I had left the Gardens, my grandfather died. This book, in part, seeks to trace the long shadow of his absence and to honor and reframe his presence. But, ultimately, it is not about him. While I hope this book sheds light on how to better care for people with dementia, my primary aim does not involve teaching techniques or methods. Rather, this book is about those of us who do not have dementia yet; those of us who never will; and those of us who are already suffering dementia’s effects or have friends or family who are. It is about examining our fears, questioning our culture, and—at least in my case—reorienting one’s spirituality in light of the challenges and possibilities such diseases bring forth. It is a book about vanishing, and what “vanishing” really means.
The skull in Vanitas Still Life, while undoubtedly grim, bears a wry, gapped grin—a grin missing four front teeth. Stripped of its flesh, our bone structure apparently discloses a faint, effortless smile. The skull’s stark, denuded presence signals gravity, but its blithe affect signals buoyancy. Perhaps this face of death reflects both the weeping Heraclitus and the laughing Democritus, pointing viewers back to Ecclesiastes: there is “a time to weep and a time to laugh.” Wisdom here comes lodged in apposition—pairs of apparent opposites, united by the word “and”: “a time to be born, and a time to die [. . .] a time to break down, and a time to build up [. . .] a time to cast away stones, and a time to gather stones together [. . .]” These lines in Ecclesiastes encourage readers to imagine a world in which the poles of existence create vibrant tension, in which life and death, gathering and releasing, embracing and refraining, weeping and laughing, do not negate each other, but instead balance and enrich. There is aggregation and integration—even with loss, even in death.
Dementia, too, invites this kind of conjunction. There is dilution and distillation, constriction and expansion, disorder and constancy. Certain aspects of persons and their relationships fade—and other dimensions crystallize, possessing a new kind of clarity. Dementia places new constraints on communication—and relationships expand to include new ways of being and loving. Cognitive changes upset the usual patterns of one’s life—and some rhythms remain unchanged.
I heard a woman describe her spouse with dementia as “my gone but not gone husband,” and her phrase seemed to strike at the heart of dementia’s paradoxes: an acute awareness of absence, and an equal insistence on presence. Lately, I am struck by its general relevance, as I consider my own gone and not-gone self. The cells that comprise my body—all of our bodies—routinely break down or slough off, and new ones take their place. Some cells, like neurons, die and are never replaced. Paradox lives at the heart of my faith, too: the gone and not-gone ego, the gone and not-gone Jesus. The play of presence and absence infuses all of life, I think, both before and after dementia.
Maybe if we can learn to inhabit this tension, this space between opposites, then dementia and the lives it touches can rejoin the spectrum of human experience, rather than being reduced to tired tropes and burdened by outsized fears, its sufferers and caregivers made to disappear. Imagine if we received all lives—those with and without dementia—as conglomerations of the ordinary and the peculiar, the fragmented and the whole, the present and the vanishing.