Читать книгу The Doulas - Mary Mahoney - Страница 11
На сайте Литреса книга снята с продажи.
ОглавлениеLook But Don’t Touch
Mary and Maria
“You can start now.” Dr. B smiles over at me expectantly as Ann snaps latex gloves on her hands and pulls them to her elbows. I move closer to the procedure table and touch its cool blue vinyl with the tips of my fingers, my other hand clenched tightly at my side. Maria’s eyes flutter open as she feels my presence.
“¿Cómo estás?” I whisper, folding my five-ten frame to be near my client.
“Bien,” she mouths back, then stares at the ceiling.
I follow her gaze and take in the room, a large rectangle, clean and open and somehow beautiful to me. At my back the entrance is concealed by a patterned curtain that circles around door, adding a layer of privacy for the client. Next to the door is a sink, the kind with foot pedals. The walls are lined with windowed cabinets, filled with the medications and medical supplies needed for a D and C, including chucks, gauze, gloves, sanitizer, antiseptic, and dozens of wrapped flexible curettes of various sizes.
The procedure table, where Maria lies, sits toward the back of the room. A white paper barrier rests between her and the slick vinyl. Her legs remain flat across the table, not yet fitted into the metal stirrups dangling at its sides. Tucked into the basket that holds the blood pressure cuff behind Maria is a box of tissues, a staple of doula care. At the foot of the table is a tray wrapped in soft, sterile cloth. I would come to know its contents well, their curves and sheen a second nature to me: dilators, clamps, sharp curettes, forceps, speculums, and long needles to reach into the cervix.
My attention rests on Ann, the head nurse, who is standing opposite me. Ann appears disinterested in me. She avoids eye contact as if she can sense I am seeking her approval, that I need something from her. I desperately want her to like me in a way that makes me feel twelve years old again, meeting my sixth grade teacher for the first time. This dynamic is established within seconds of my arrival, and in a way, Ann does become one of my teachers.
As I hover awkwardly near Maria, I realize I know very little about her. This unsettles me. I imagine the next fifteen minutes to be intimate, overwhelming. We are bound together by a few square feet; our bodies nearly touch, we breathe the same air. We had met briefly during precounseling earlier in the week, yet my mind at this point is a sea of facts and faces, times and names. My own ego swims and splashes through them all until my eyes are squinted and blurred, and I can only see myself pooled at the center.
Pop music plays softly on the portable radio, and Dr. B’s metal instruments clink on the procedure tray as Maria breathes deeply at my side. This combination of sounds would become a part of my being as a doula. Warm morning sun pours through a picture window and down onto my client and me. The blinds are raised, revealing a fifteen-story drop, and I watch the cars multiply on the highway outside, stuck in the Manhattan commute. The river flows just beyond, and I try to make out the silhouette of my own apartment building on the other side in Brooklyn. I picture myself tonight on my roof under the sticky August moon looking back at City Hospital.
I stand above Maria, unsure of my next move. To say that my mind went blank would imply that I had some sort of plan that I had momentarily forgotten. But there isn’t a plan, not really. Only a purpose: to help this woman feel safe and supported during her abortion. Whether or not I know how to do that, I am about to find out.
“I’m a doula.”
“A what?”
“A doo-lah.”
“Huh?”
“D-o-u-l-a. I attend births and abortions.”
“Oh! Wow! That’s amazing!”
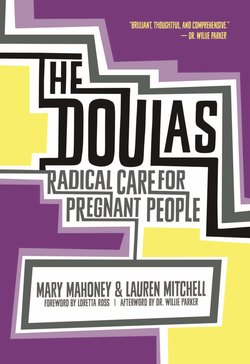
So have begun many conversations in the lives of full-spectrum doulas. While doulas are all Lauren and I have thought about for the better part of the last decade, we are never surprised when we meet someone who has never heard of them. Even in 2016, many small towns and big cities still have no knowledge of or access to doulas. We attribute this in part to the abysmal state of reproductive healthcare in our country, the dearth of resources available for women to have an empowered and woman-centered pregnancy experience. More than that, we believe it is reflective of how society feels about women, about what they deserve and don’t deserve—especially when pregnant.
Pregnant people are not to be trusted. This message is deeply ingrained in our culture. It’s everywhere: in our laws, in our media outlets, in our homes. It’s rooted in the patriarchal fear of female power and sexuality, and its pervasiveness reaches into the psyches of women themselves.
I can relate. Coming of age in white, working-class southern Indiana, a swath of the country where conservative roots grow into all its children—long before the Religious Freedom Restoration Act and Purvi Patela—I was terrified of anything having to do with sex or my body. With good reason I thought: I could get pregnant. And that would be the worst thing that ever happened to me; pregnant girls dropped out of school and stayed in Smalltown, Indiana.
In the spring of 1995 I sat in my seventh grade health class, attention rapt as two high school seniors, a girl and a boy, gave me my first lesson in sex. She played varsity volleyball and had dated my friend’s older brother. Her skin glowed gold as though she had just emerged from a tanning bed, and thin blond streaks ran through dark, gelled hair. Her raspy voice was confident and a little bored, as if she’d had this conversation a million times before. “Sex,” she began with authority. He wore a letterman’s jacket and didn’t say much.
My best friend Meredith sat next to me, passing notes and rolling her eyes. Meredith already knew about sex, at least theoretically. She’d had boyfriends for years. She was “wanted.” I was completely virginal and had only gotten my period that summer. At its inauguration Meredith had been over, and we sat on the edge of my claw-foot tub in the upstairs bathroom—door locked—while she told me about tampons. I was horrified at the thought of sticking something in my vagina. I went to find my mom. She gave me a big hug and an even bigger pad. Meredith took me for a walk to try to ease the cramps, the giant pad making a deafening noise with each step. We passed by the houses of boys we had crushes on. She was always appalled by my choices in love: “Mary! No!” Even with my latest crimson leap into “womanhood” we both knew they would never be more than a fantasy: I was not having sex.
There was a singular view of premarital sex in my hometown: Don’t do it. That’s what the high school seniors were preaching on this sunny day in southern Indiana: “You are worth waiting for!” They gave me a sticker to prove it. I eagerly stuck it to the cover of my notebook.
This message of abstinence hovered over my Christian community, a town that became quiet as a ghost on Sunday mornings. I myself went to worship the Lord every now and then. My mom even taught Sunday school to the pre-K crowd at a stuffy church attended by the hundred or so rich people in our town—but mostly she did it to throw an extra twenty-five bucks a week in our family coffer. In church, God was the one whispering, “No premarital sex.” I don’t remember ever thinking much about God. If anything, I wasn’t a fan because he reminded me of the way the snooty old ladies in pews looked down on me, my brother, and my sister. I had no idea at the time that a big part of my adulthood would be dedicated to navigating God and spirituality as a doula.
As the years passed, I learned I was far from a “good girl.” I had run drunkenly from the cops through my fair share of cornfields, smoked cigarettes on the floor of my car during lunch period. But God or no God, sex still scared me. Sexually transmitted diseases? Pregnancy? Getting stuck in Indiana? I chose to keep my legs tightly closed.
By the time I was a high school junior, it was 1998 and the welfare reform law had set in motion an abstinence-only campaign valued at $50 million per year. In other words, still no premarital sex—no how, no way. I became a “Lifesaver,” along with many of my friends. We went from class to class and school to school, showing photos of genital herpes and pregnant teenagers to underclassman. “Do NOT have sex!” we told them gravely. The words abortion, birth control, and even birth were never uttered. (Not long into the program, rumors started flying that several of the Lifesavers were giving blow jobs, among other activities. It became difficult for anyone to take us seriously.)
My parents ignored the Lifesavers aspect of my school life. If anything they were confused. They were former hippies, rare liberal birds from “up North.” “You’re a feminist!” my dad would tell me. I didn’t experience his claim as a compliment. I was convinced my dad just thought I was too opinionated or weird or bitchy. I had no concept of feminism at that point. It just wasn’t part of the vocabulary of my youth.
Meanwhile, Meredith and I drifted apart. She got a serious boyfriend, and I began socializing with the “party” crowd. The night of high school graduation we got together to go to one last party. Despite my loathing for my hometown, money was tight, and I was planning to stick around for a few more years, live with my dad, work my minimum wage job as a Subway “sandwich artist,” and attend community college. Meredith was off to Purdue. She couldn’t wait to get out of there. “I fucking hate this place!” she yelled. Our car was a whizzing dot on the high school’s security cameras. I was sitting next to her smoking, silently sticking my middle finger out the passenger window.
We didn’t see each other again that summer. I got a call from her halfway through spring semester of our freshman year: “I’m pregnant. I’m coming back home.” We spent the next six months watching Felicity, eating ice cream, and being best friends again. Meredith was having the baby, unlike another friend of ours, Shannon, who was also pregnant.
I met with Shannon over a keg of beer at a party on the lake. “I had an abortion today,” she said, drinking from her foamy cup.
I stared at her. “Are you okay?”
She shrugged. “Yeah.”
I went back over to my group of friends to gossip. “And she’s here,” I told them, “drinking beer!” We looked on in horror.
Dr. B injects fentanyl and Versed into the IV on Maria’s right arm. “This will make you more comfortable and relaxed, like a few cocktails,” she explains to Maria, winking at me. I realize I should have done more research before coming into the room. On the procedure, on the meds they’re using, on the exact moments Maria might need me most.
The truth is, Lauren and I have kind of been winging it since we partnered with City Hospital last week, still not believing—after months of being shut down by other clinics—that they actually wanted abortion doulas in this room. We’ve been more focused on the logistical rush: getting time off work, meeting the clinicians and counselors, figuring out how to get from one room to the next in the hospital’s maze of corridors. (As we grew our organization, we would find that a combination of “winging it,” just jumping the hell in with both feet, and meticulously scheduling ourselves would get us through many days.)
My background is in research and development; I’ve never done anything that even hints at direct care. The design of this project has been strictly theoretical up to this point, mostly speaking at conferences about the model with bits and pieces of clinical intelligence from Lauren’s brief stint at a birth center. The closest I’ve been to an abortion was sitting in the waiting room at Planned Parenthood while a friend went behind closed doors, coming out hours later no longer pregnant. Even though I had trained as a birth doula the year before, I had yet to attend a birth. And anyway, how do you prepare for something that hasn’t existed in this exact form before, at least as far as we knew? What exactly was an abortion doula? What did I need to learn?
One thing I would learn is that the process of undergoing a procedure that is only five to seven minutes in length can become a complicated, jagged puzzle our clients have to put together, often in isolation. Each puzzle piece represented a decision our client would make along the way, sedation selection being only one of these pieces.
The “cocktail” metaphor Dr. B used described the sensation of the client becoming more relaxed and drowsy due to her anxiety level being reduced and her physical pain being alleviated by the medication. This sounded great to me. Who wouldn’t want this to be her experience of abortion? I would just as quickly see some of the drawbacks of this type of sedation, however. The client’s memory of the procedure would be negligible in many cases. For those wanting a more embodied experience of the abortion, this would be problematic. Not to mention, the more drugs used, the higher the cost in most clinics. Recovery time would also be extended and a personal escort would be required to take a client home from the abortion. Again, problematic for anyone who could not spare more time than the abortion itself required, or for people who could not or would not tell a family member or friend to meet them at the clinic after.
I wonder who Maria’s support person is, who will be taking her home from her abortion. My eyes shift back and forth between her and the foot of the bed where Dr. B is reviewing the finer points of the procedure with Dr. W, a resident who started her rotation a few weeks ago. They turn to face us. “Okay, Maria, I’m going to do a pelvic exam now. Open your legs until you feel the sides of my hands,” Dr. W says gently in Spanish.
Maria winces at the pressure of the exam. Shit, what do I do? I quickly flash back to my birth doula training, looking for guidance. “No, no, no, not like this. You want to hold her like this,” my trainer had yelled. “You need to build up the muscle in those upper arms!” Not helpful. I shake the memory from my head. I’m unsure of how I fit into this space, surrounded by “experts.” It’s one of the most common feelings for any new doula until we realize we aren’t supposed to be experts; our clients don’t need another expert in the room.
Ann grabs Maria’s hand and nods at me to do the same, sensing my panic. “Respire profundo, respire profundo,” she coaches Maria and me.
“Respire,” I whisper, smiling at Ann gratefully and reaching for Maria’s left hand with both of mine. Much of what we would learn about compassionate care would come from observing nurses and counselors.
Maria grips my hands hard and nods, inhaling and exhaling, her eyes locked into mine. I feel breathless at the intimacy of her gaze. I have typically shied away from intimacy with strangers and loved ones alike. For most of my time on earth, I may as well have been wearing a sign around my neck with the words, “You can look, but you can’t touch.”
But in this moment, looking into Maria’s eyes, something clicks, and I suddenly know what to do, as though the ability to care for another person has always been inside of me, dormant. My senses heighten as I begin to tune into my role, to be in two places at once, the head of the bed and the foot of the bed. I am acutely aware of the client’s every breath and the doctor’s every movement.
A sheet over Maria’s knees offers me only a partial view of the procedure that I would come to know by heart. Betadine, an antiseptic, is smoothed onto the vagina, vulva, the upper thighs, and abdomen with a sponge. The speculum is placed and secured, followed by an injection of lidocaine into the cervix. The tenaculum is clamped and the metal cannula is inserted in progressive sizes until the cervix is properly dilated. I find myself mesmerized by the elegance of Dr. W’s motions, her wrists and fingers moving with the grace of a pianist.
Maria is groggy. She drifts in and out of consciousness, occasionally waking with quick, sharp breaths. I continue to hold her hand in mine, trying to anticipate what she might need. Dr. W selects a flexible curette, measured for Maria’s current number of gestational weeks. She tests its size in Maria’s cervix and attaches it to the Manual Vacuum Aspirator, a tool I had once seen on a tour of Ipas—its manufacturer—in North Carolina. Dr. W presses the buttons on the side of the MVA to release the vacuum as she moves it in 180-degree angles, an in-and-out motion, feeling for the “gritty sensation” that indicates the pregnancy has been removed. Maria’s moans intensify as she shifts on the table, her uterus contracting.
“Este es el último paso,” Dr. W tells us. I look over at the clock. It’s been less than ten minutes. I brush the perspiration from Maria’s face with a tissue. Her eyes are tightly closed now as she hums through what is typically the most physically difficult part of the procedure.
“Fin,” the doctor says anticlimactically. She deftly removes the speculum and folds the instruments back into the sheet. Dr. B leaves the room with the products of conception.
Maria has opened her eyes, our damp hands entwined. I’m not sure if it’s her sweat or mine. “Gracias,” she says in a tone that makes me feel as if I have just won an award, though for what I’m not exactly sure. Didn’t I just stand there? Wouldn’t she have been fine without me?
It would take me many more abortions, many more conversations, and hours of internal reflection to learn how profound the doula role is: how “just being there,” a silent observer, bearing witness to someone else’s experience and reflecting it back to them can be so much and enough. Critics and supporters alike would sometimes claim the abortion doula role to be sensational or unnecessary. They would miss the bigger point and strip the entire experience of its greater meaning.
“De nada,” I smile back, offering Maria the rest of the Spanish that I know.
Dr. B reenters and quietly tells Dr. W that the pregnancy has been removed completely. Maria can go to recovery now. Ann eases her into the recliner, discreetly tossing the blood-soaked plastic chuck underneath her into the wastebin.
We wave goodbye.
As a reproductive justice activist for more than a decade, I have often been asked how I got into this work, what inspired me, and why doula care? These have been tough questions to answer. For years I avoided sharing my abstinence-only background, my fear of sex, the time I publicly shamed a friend for having an abortion. I thought that if I didn’t fit into a perfect activist box I would be cast out of the movement.
When I started talking, though, I learned my story was more common than I thought—maybe the most common of all stories. Most women in the United States have to confront the fear we have of our own bodies and sexuality and how we project that onto others and internalize it within ourselves. When I was growing up, no one ever spoke to me in a real way about my body or my health—not even my staunchly pro-choice, hippie parents. When I ask my parents about this now, my dad shrugs wistfully, “But I thought you weren’t having sex.” My mom, who has always welcomed any and every topic under the sun, simply says, “I didn’t know how to talk about it.” They aren’t alone; most parents don’t know how to talk to their kids about sex. Conversation around abortion and birth in my community was not nuanced—there was no conversation at all. That inane and dangerous “Lifesavers” program was the only vehicle my classmates and I had to talk about or to be close to sex. We all just wanted to explore something innate and undiscovered in ourselves.
I’ve stopped being ashamed of my story. Mostly. It led me to doula work. Being a doula speaks directly to the part of myself that is complex and contradictory, and it doesn’t let me hide from it. It allows me to juxtapose two opposing ideas and say these are not bad or good—they just are. It opens up a space for things to be messy, unpackaged, raw, unflinchingly human. When I work with a client, I become an activist in a way I didn’t know was possible. There is no box I have to fit into.
After I witnessed that first abortion, I was on fire, more alive than I’d ever been. I felt as if I was part of some sort of historical moment. I wasn’t. Abortions happen every day—more than a million people have abortions every year in the United States alone. But witnessing the care and being part of the care that goes into the abortion experience was something I wasn’t aware of before. At least not in the way I saw at the hospital that day from the doctors and nurses, and even from myself. I wanted to tell the world about this care. I wanted to capture it in a bottle and pour it over everyone who would ever have an abortion.
This would prove to be difficult. Many cities would not see the value of abortion doula care. Many pregnant people would not have access to the kind of abortion care they wanted or needed. As we expanded our work, the privilege our clients held just by virtue of the fact that they were in New York City became clear. Here, abortion is accessible up to twenty-four weeks, Medicaid covers most procedures, and there are several options for care, from at-home medical abortion to freestanding clinic abortion to hospital-based abortion. Our clients don’t encounter the restrictions on abortion that people in other states face, such as mandated waiting periods, consent requirements, or unreasonable travel barriers. Our fellow doulas around the country would struggle against these restrictions and many would be denied the opportunity to ever get into a clinic.
And yet we would find, for our clients in New York City, the emotional experience of abortion often transcends many of these legal barriers. Years later Dr. B reflects on the early days of the Doula Project:
Mostly I remember being really grateful that you were there because patients had an enormous amount of anxiety. Even though in New York City you don’t always have to walk through a thick line of protesters, I think that most people who have abortions have ambivalent feelings about it. Sometimes it’s a very intense, very painful part of their lives. And having somebody to attend to emotional needs and just be there and hold their hands made a huge difference in the quality of [care]. I remember [the doulas] at the head of the bed while performing procedures and really providing a lot of comfort. And that was huge. I remember watching you guys getting so attached to these people, which . . . was really touching.
The deeply collective nature of the world we would help create within the clinic walls started to show itself to me that first week. Before we entered City Hospital we imagined ourselves as totally client focused. Birth doulas, at the time, frequently held contentious relationships with labor and delivery staff, and we were prepared for a similar experience in the clinics. Yet the impact we would have on the doctors and nurses who served our clients would become a cornerstone of our mission. Dr. B remembers, “You made a big difference for people. In addition to [the patients], as a young provider, as I was at the time, it’s really nice to have validation. The group of [doulas] was so kind to us as providers. You know, abortion providers don’t get that much love in the world, but we got so much love and respect from you. That was really lovely.”
The Doula Project would become the most rewarding work of my life, but it would never be without its hardship or stigma. It was not work I could share with my Christian community in southern Indiana. (To this day I can count on one hand the number of times I’ve said the word “abortion” outside the walls of my parents’ homes. Meredith and I continue to lock ourselves behind closed doors—talking in hushed tones about anything “vagina related.”) The fire I felt the first days and weeks and months would burn out, and I would come to carry a certain amount of pain and dread with me. My clients would change me, how I practice care and walk through the world. The abortions, the stillbirth inductions, the adoption plans, they would move into me, and I would hold on to tiny pieces of every person I cared for.
Fellow doula and energy healer Jini Tanenhaus would later tell me, “Your chakras are closed around your heart. That’s very common in this line of work. You’re heartbroken.” Caregiving leaves a mark. And who cares for the caregiver? Who do we let care for us? Though Lauren and I would often pride ourselves on being “hardcore,” unsentimental to the point of detachment, deep down we also needed someone to care for us. Like many caregivers, we—as well as the doulas in the stories that follow—would struggle to allow ourselves to be vulnerable in that way, to let others see us when we were scared or tender, even as we levied that brand of care to our clients and to the world.
Maria was the first—the first client in an organization that would go on to support more than thirty-five thousand people across the spectrum of pregnancy options over the next decade.
a Religious Freedom Restoration Act: an Indiana Senate bill signed into law in 2015 that, in a nutshell, asserts that individuals and companies may use their religion as a defense in denying services to others. The LGBTQ community has been particularly targeted by this law. Purvi Patel: a pregnant woman who was charged with feticide and child neglect and sentenced to twenty years in prison for allegedly inducing her own miscarriage.