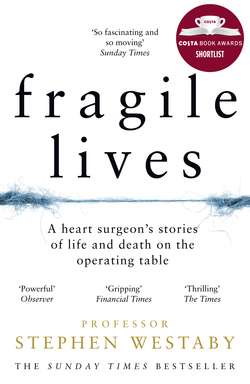
Читать книгу Fragile Lives: A Heart Surgeon’s Stories of Life and Death on the Operating Table - Stephen Westaby, Stephen Westaby - Страница 9
the ether dome
ОглавлениеFor this relief much thanks; ’tis bitter cold and I am sick at heart.
William Shakespeare, Hamlet, Act I, Scene i
The finest of margins separates life from death, triumph from defeat, hope from despair – a few more dead muscle cells, a fraction more lactic acid in the blood, a little extra swelling of the brain. Grim Reaper perches on every surgeon’s shoulder and death is always definitive. There are no second chances.
November 1966. I’m eighteen and a week into my first term as a student at the Charing Cross Hospital Medical School in the centre of London, just across from the hospital itself. I wanted to see a vibrant, beating heart, not a slimy piece of lifeless meat on the dissection table. I was told by a hall porter at the school that heart surgery was done over the road in the hospital on Wednesdays and that I should look for the ether dome. Find the green door on the very top floor under the eaves where nobody goes. But don’t get caught, he warned me. Pre-clinical students are not allowed up there.
It was late in the afternoon, already dark, and drizzle was falling on the Strand when I set out to find the ether dome, which turned out to be an antiquated leaden glass dome above the operating theatre in the old Charing Cross Hospital. Not since my entrance interview had I entered the hallowed portals of the hospital itself. We students had to earn that privilege by passing exams in anatomy, physiology and biochemistry. So I didn’t enter by the Grecian portico of the main entrance, but sneaked in through Casualty under the blue light and found a lift, a rickety old cage used to take equipment and bodies from the wards to the basement.
I worried that I would be too late, that the operation would be finished – and that the green door would be locked. But it wasn’t. Behind the green door was a dark, dusty corridor, a depository for obsolete anaesthetic machines and discarded surgical instruments. Ten yards away I could see the glow of the operating lights beneath the dome itself. It was an old operating theatre viewing gallery respectfully separated by glass from the drama on the operating table no more than ten feet below, with a hand rail and curved wooden benches worn smooth by the restless backsides of would-be surgeons.
I sat clutching the hand rail, just me and Grim Reaper, and peered through glass hazy with condensation. It was a heart operation and the chest was still open. I moved to find the best view, settling for a position directly above the surgeon’s head. He was well known, at least in our medical school, a tall man, slim and imposing, with very long fingers. In the 1960s heart surgery was still new and exciting, its practitioners few and far between, and not many had been properly trained in the specialty. Often they were skilled general surgeons who had visited one of the pioneering centres and then volunteered to start a new programme. They were on a steep learning curve, with the cost measured in human lives.
The two surgical assistants and the scrub nurse were huddled together over the gaping wound, frantically shuttling instruments between them. And there it was, the focus of their attention and of my fascination. A beating human heart. In fact it was squirming more than beating, and was still attached by cannulas and tubing to the heart–lung machine. Cylindrical discs were spinning through a trough of blood bathed in oxygen and a crude roller pump squeezed the tubes, accelerating this life blood back to the body. I peered closer but could only see the heart as the patient was completely covered by green drapes, gratifyingly anonymous to all concerned.
The surgeon restlessly shifted his weight from foot to foot, wearing the big, white operating boots that surgeons once used to keep blood off their socks. The team had replaced the patient’s mitral valve but the heart was struggling to separate from the bypass machine. This was the first time I’d seen a beating human heart, and even to me it looked feeble, blown up like a balloon, pulsating but not pumping. On the wall behind me was a box marked ‘Intercom’. I threw the switch and the drama now had a soundtrack.
Against the din of amplified background noise I heard the surgeon say, ‘Let’s give it one last go. Increase the adrenaline. Ventilate and let’s try to come off.’
There was silence as everyone watched the desperate organ fight for its life.
‘There’s air in the right coronary,’ the first assistant said. ‘Give me an air needle.’ He shoved the needle into the aorta, frothy blood fizzed into the wound, then the patient’s blood pressure started to improve.
Sensing a window of opportunity, the surgeon turned to the perfusionist. ‘Come off now! This is our last chance.’
‘Off bypass,’ came the reply, said more as a blunt matter of fact than with any great confidence.
The heart–lung machine was switched off and the heart was now free-standing, with the left ventricle pumping blood to the body, the right ventricle to the lungs. Both were struggling. The anaesthetist stared hopefully at the screen, watching the blood pressure and heart rate. Knowing that this was their last attempt, the surgeons silently withdrew the cannulas from the heart and sewed up the holes, each one of them willing it to get stronger. For a while it fluttered feebly but then the pressure slowly drifted down. There was bleeding from somewhere – not torrential but persistent. Somewhere at the back. Somewhere inaccessible.
Lifting the heart caused it to fibrillate. It was now squirming again, wriggling like a bag of worms, but not contracting, fed by uncoordinated electrical activity. Wasted energy. It took the anaesthetist a while to spot this on his screen. ‘VF,’ he shouted. I’d soon learn that this meant ventricular fibrillation. ‘Shock it.’
The surgeon was expecting this and was holding the defibrillating paddles hard against the heart. ‘Thirty joules.’ Zap! No change. ‘Give it sixty.’
Zap! This time it defibrillated, but then just sat there stunned and devoid of electrical activity, like a wet brown paper bag. Asystole, as we call it.
Blood continued to fill the chest and the surgeon poked the heart with his finger. The ventricles responded by contracting. He poked it again and the rhythm returned. ‘Too slow. Give me a syringe of adrenaline.’ The needle was shoved unceremoniously through the right ventricle into the left, and a clear liquid squirted in. Then he massaged the heart with his long fingers to push the powerful stimulant into the coronary arteries.
The grateful heart muscle responded rapidly. Straight out of the textbook, the heart rate accelerated and the blood pressure soared, up and up, dangerously testing the stitches. Then, as if in slow motion, the cannula site in the aorta gave way. Whoosh! Like a geyser erupting, a crimson fountain hit the operating lights, spraying the surgeons and soaking the green drapes. Someone murmured, ‘Oh, shit.’ An understatement. The battle was lost.
Before a finger could plug the hole the heart was empty. Blood dripped from the lights and red rivulets streamed across the marble floor. Rubber soles stuck to it. The anaesthetist frantically squeezed bags of blood into the veins, but to no avail. Life was fast ebbing away. As the injected slug of adrenaline wore off, the turgid heart simply blew up like a balloon and stopped. Stopped forever.
The surgeons stood silently in despair, as they did week after week. The senior surgeon then walked away out of my view and the anaesthetist turned off the ventilator, waiting for the electrocardiogram to flatline. He removed the tube from the patient’s windpipe, then he too disappeared from view. The brain was already dead.
Just yards away mist descended on the Strand. Commuters rushed into Charing Cross Station to get out of the rain, late lunches were finishing at Simpson’s and Rules, cocktails were being shaken in the Waldorf and the Savoy. That was life, this was death. A lonely death on the operating table. No more pain, no more breathlessness, no more love, no more hate. No more anything.
The perfusionist wheeled his machine out of theatre, and it would take hours to disassemble, clean, restore and sterilise it for the next patient. Only the scrub nurse lingered. Then she was joined by the anaesthetic nurse who had comforted the patient in the anteroom. They took off their masks and stood silently for a while, unconcerned by the sticky blood that covered every surface and by the chest still splinted open. The anaesthetic nurse searched for the patient’s hand beneath the drapes and held it. The scrub nurse pulled away the blood-soaked covering from the face and stroked it. I could see the patient was a young woman.
They were oblivious to the fact that I was upstairs in the ether dome. No one had seen me there. Only Grim Reaper – and he’d already departed with the soul. I gingerly shifted along the bench to look at the woman’s face. Her eyes were wide open, staring up into the dome. She was ashen white but still beautiful, with her fine cheek bones and jet black hair.
Like the nurses I couldn’t leave. I needed to know what happened next. They peeled back the bloodied drapes from her naked body. I was silently screaming for them to take out that hideous retractor cranking open her breastbone and let her poor heart go back to where it belonged. When they did the ribs recoiled and the poor lifeless organ was covered again. It lay flat, empty and defeated in its own space, with just a fearsome, deep gash separating her swollen breasts.
The intercom was still switched on and the nurses started to talk.
‘What’ll happen to her baby?’
‘Adopted, I guess. She wasn’t married. Her parents were killed in the Blitz.’
‘Where did she live?’
‘Whitechapel, but I’m not sure the London do heart surgery yet. She got really sick during the pregnancy. Rheumatic fever. She nearly died during the delivery. Might’ve been for the best.’
‘Where’s the baby now?’
‘On the ward, I think. Matron’ll have to deal with it.’
‘Does she know?’
‘Not yet. You go and find her. I’ll get some help to finish off.’
It was all so matter of fact. A young woman had died, her baby left without a relative in the world. No more love, no more warmth, lost amid that tangled, blood-soaked technology in the operating theatre. Was I ready for this? Was this what I aspired to?
Two student nurses came to wash the body. I recognised them as respectful public schoolgirls from the Friday-night freshers’ dance. They’d brought a bucket of soapy water with sponges and set about scrubbing her clean. They removed the vascular cannulas and the bladder catheter but were visibly upset by the wound and what lay beneath. Blood kept slopping out of it.
‘What did she have done?’ asked the girl I’d danced with.
‘Heart operation, obviously,’ came the reply. ‘Valve replacement, I guess. Poor kid. She’s only our age. Bet her mum’s upset.’
They covered the wound with gauze to soak the blood, then taped it up. The scrub nurse returned and thanked the girls for a job well done. She called back the surgical registrar to close over the wound, ready to move the body to the mortuary, as all deaths on the operating table are referred to the coroner for autopsy. The young woman would be sliced open again from neck to pubis, so there was no point closing the breastbone or bringing together the different layers of the chest wall. He took a big needle and some thick braid, and sewed her up like a mail bag. The wound edges still gaped and oozed serum. Mail bags were much neater.
It was now around 6.30 in the evening and I was meant to be in the pub down the road getting pissed with the rugby team. But I still couldn’t leave. I was attached to this empty shell, this skinny corpse I’d never met but now felt I knew well. I’d been with her at the single most important part of her life.
The three nurses manhandled her into a starched white shroud with a ruff around the neck, tied it up at the back then secured her ankles with a bandage. She was beginning to stiffen with rigor mortis. The students had done their job with kindness and respect. I knew that I would meet them again. Maybe I’d ask them how they felt.
Now there were just the two of us left, the corpse and me. The operating lights still shone on her face and she was staring straight up at me. Why hadn’t they closed her eyelids like they did in the movies? I could see through those dilated pupils to the pain etched on her brain.
From fragments of conversation I’d overheard and with just a little medical knowledge I could sketch her life story. She was in her twenties. Born in the East End. She could only have been a small child when her parents were killed in the bombing. As a child she carried the scars of those sights and sounds, the fear of being alone as her world disintegrated. Brought up in poverty, she develops rheumatic fever, a simple streptococcal sore throat that triggers a devastating inflammatory process. Rheumatic fever was common in areas of deprivation and overcrowding. Perhaps she had painful, swollen joints for a few weeks. What she doesn’t know is that the same inflammation is in her heart valves. There was no diagnostic test in those days.
She develops chronic rheumatic heart disease and is known as a sickly child. Perhaps she develops rheumatic chorea – involuntary, jerky movements, unsteady gait and emotional turmoil. She gets pregnant, an occupational hazard. But this makes things worse as her sick heart must work much harder. She becomes breathless and swollen but makes it through to term. Maybe the London Hospital delivers her safely but recognises heart failure. A murmur. A leaking mitral valve. They prescribe the heart drug digoxin to make it beat stronger, but she doesn’t take it as it makes her nauseous. Soon she’s too tired and breathless to look after the baby, and she cannot lie flat. With worsening heart failure her outlook is grim. They send her to the city to see a surgeon, a real gentleman in a morning suit with pinstriped trousers. He’s kind and sympathetic, and says that only surgery on her mitral valve can help. But it doesn’t. It terminates her sad life and leaves another orphan in the East End.
When the porters came for her the operating lights had long been switched off. The mortuary trolley – a tin coffin on wheels – was drawn up alongside the operating table. By now her limbs were rigid. The body was unceremoniously dragged into this human sardine can, her head bouncing with a sickening thud, but nothing could hurt her any more. I was relieved to lose eye contact. A green woollen blanket was folded over the top to make it look like an ordinary trolley, and then off they went to slot her into the fridge. Her baby would never see her again, would never have a mother again.
Welcome to cardiac surgery.
I sat there, arms on the rail, chin on my hands, staring down from the ether dome at the black rubber surface of the empty operating table, as generations of would-be surgeons had done before me. The ether dome was a gladiatorial amphitheatre, people coming here to gaze down on a spectacle of life or death. Perhaps if others had been there it might have seemed less brutal, others with whom to share the shock of this poor girl’s death, the misery awaiting her child.
Auxiliary nurses came with mops and buckets to erase the last traces of her – her blood now dry on the floor around the operating table, the bloody footprints heading towards the door, the blood on the anaesthetic machine, the blood on the operating lights. Blood everywhere – now meticulously wiped up. A slip of a girl reaching up to clean the operating light saw me in the dome, my pale face and staring eyes against the gloom. I frightened her, and so it was my cue to leave. But one spot of blood remained on top of the light where no one could see. Adherent and black, it said part of me is still here. Remember me.
The green door closed behind me and I walked away to the shuddering lift where her body had been taken down to lie in a cold fridge in the mortuary.
Notice of autopsies were posted on a board in the entrance hall of the medical school. Usually the patients were elderly. The young ones were either drug addicts, road-traffic accidents, suicides from the underground system or cardiac surgery patients. I found her on the list for Friday morning. She was called Beth. Not Elizabeth, just Beth. She was twenty-six years old. It had to be her. On the day of the autopsy the bodies were brought from the hospital mortuary in the basement, then dragged under the road to the medical school in a tin box on rails by a pulley system and up the lift to the autopsy room. Should I go? Should I watch her guts and brain be cut out, watch her dead heart be carved into slices, tell them how she really died in that crimson fountain?
No, I couldn’t do it.
Beth taught me a very important lesson that day in the ether dome. Never get involved. Walk away as her surgeons did and try again tomorrow. Sir Russell Brock, the most renowned heart surgeon of the era, was known for his bluntness about losing patients – ‘I have three patients on my operating list today. I wonder which one will survive.’ This may seem insensitive, even callous, but to dwell on death was a dreadful mistake then, and it still is now. We must learn from failure and try to do better the next time. But to indulge in sorrow or regret brings unsustainable misery.
I grappled with this later in my career when my interests veered towards the sharp end: heart surgery for complex congenital anomalies in babies and young children. Some came toddling happily into the hospital, teddy bear in one hand, Mummy holding the other. Blue lips, little chest heaving, blood as thick as treacle. They’d never known a different life and I strived to provide that for them. To make them pink and energetic, liberate them from impending doom. I did this in good faith, yet sometimes without success. So what should I do? Sit with the weeping parents in a dark mortuary holding a cold, lifeless hand, blaming myself for taking that risk?
All heart surgery is a risk. Those of us who make it as surgeons don’t look back. We move on to the next patient, always expecting the outcome to be better, never doubting it.