Читать книгу Essential Cases in Head and Neck Oncology - Группа авторов - Страница 58
Management
ОглавлениеQuestion: Which of the following imaging studies would be appropriate next steps in the evaluation and management of this patient?
A CT of the neck and chest with IV contrast: yes/no. This is a potential next step as this will allow for evaluation of the neck and the upper aerodigestive tract. CT chest will complete the metastatic workup. CT images are rapidly obtained and provide both soft tissue and bone detail. For patients being considered for transoral robotic resection, it is important to evaluate for a retropharyngeal carotid artery.
Neck ultrasound: yes/no. Neck ultrasound may be helpful here to assess for pathologic cervical lymphadenopathy and to assist with FNA, if needed. Newer techniques have also been described using transcervical ultrasound to assess for primary tumors of the palatine and lingual tonsil tissue. If a CT of the neck is performed, neck ultrasound would likely provide little additional benefit.
MRI of the neck: yes/no. This is a potential next step as this will allow for evaluation of the neck and the upper aerodigestive tract. MRI is particularly helpful in assessing for soft tissue extension to the base of tongue and/or the parapharyngeal space.
PET/CT neck: yes/no. This is a potential next step as this will allow for evaluation of the neck and the upper aerodigestive tract as well as provide assessment for metastatic disease. This study should typically be performed after confirming the presence of a malignancy.
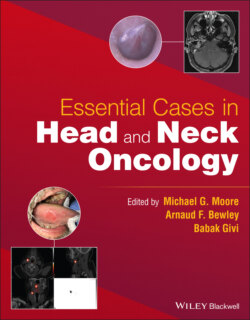
A neck CT with IV contrast and PET/CT are both performed that show a 2.5 × 1.5 cm PET avid mass in the right tonsil with involvement of the right medial pterygoid muscle (see Figure 8.1). There is no suspicious cervical lymphadenopathy or evidence of distant disease.
Question: What is the clinical stage of this patient?
Answer: cT4N0M0. The involvement of the pterygoid musculature seen on the CT and his evolving trismus make this clinically a T4 tumor using the AJCC 8th Edition staging for HPV+ oropharyngeal tumors.
Question: What would be the most appropriate treatment option for this patient?
Answer: This is not a primary tumor best approached using transoral robotic surgery (TORS) for two reasons: (i) With the advanced nature of this tumor, and extension to the pterygoid musculature, obtaining a clean resection with negative margins is very challenging unless an open approach is used: (ii) this disease likely extends beyond the superior constrictor muscle, as evidenced by the effacement of the parapharyngeal fat plane. Negative surgical margins are important to consider in this setting because postoperative adjuvant therapy for positive resection margins warrants consideration of concurrent chemoradiotherapy – which commits the patient to a trimodality approach for therapy. While a traditional mandibular split approach will allow complete access to the tumor, this approach has its own morbidity, and due to the extent of the disease, postoperative radiation therapy is still required.
Question: What is the first line treatment plan for nonoperative disease in this scenario?
Answer: Radiotherapy with concurrent bolus cisplatin (dose: 100 mg/m2 IV every 21 days for three cycles). For locoregionally advanced cancers of the oropharynx treated nonoperatively, concurrent chemoradiotherapy remains the standard of care. Cisplatin is a potent radiosensitizer. The MACH‐NC meta‐analysis clarified the survival benefit of a combined chemoradiation approach with greater benefit for platinum‐containing chemotherapies.
The bolus schedule (every 3 weeks at higher dosing), however, more than doubles the risk of severe toxicities including mucositis, fibrosis, nausea and vomiting. It has been shown that increased toxicity occurs when cumulative dosing reaches 200–300 mg/m2. To limit the toxicities of cisplatin, a weekly schedule has been adopted by many. Prospective data by Noronha et al. (2018) comparing weekly and bolus schedules demonstrated that a weekly schedule (30 mg/m2, as opposed to 40 mg/m2) was inferior in terms of locoregional control. Many institutions in the United States and Europe use 40 mg/m2 weekly, and retrospective data support similar response rates to bolus dosing with fewer toxicities. This is still an active area of study as there are no prospective studies comparing a bolus schedule to 40 mg/m2 weekly dosing.
FIGURE 8.1 These axial images of the fused PET/CT (left) and CT of the neck with IV contrast (right) demonstrate a right‐sided tonsillar mass with involvement of the right medial pterygoid muscle.
While radiotherapy with concurrent cetuximab was previously considered an appropriate alternative to cisplatin among platinum‐ineligible patients, RTOG 1016 and the European De‐ESCALaTE HPV studies both demonstrated the superiority of cisplatin in low‐risk, locoregionally advanced HPV+ oropharyngeal cancer patients, with improved overall survival and locoregional control rates with platinum compared to EGFR inhibitor therapy.
The use of pembrolizumab is indicated in unresectable locoregionally recurrent head and neck cancer and/or distant metastatic disease. Its mechanism is to bind to the PD‐1 receptors on lymphocytes to disrupt the local immune‐suppression generated by the cancer. The use of immunotherapy in the primary treatment of cancer is an area of active investigation.
Following definitive chemoradiation therapy, a post‐treatment PET/CT was performed 12 weeks after completion of treatment showing no evidence of local, regional or distant disease. The patient was started on regular surveillance follow‐up with visits every 3 months.