Читать книгу Clinical Guide to Oral Diseases - Crispian Scully - Страница 17
Case 1.3
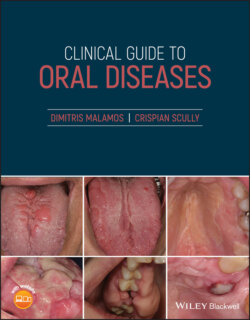
ОглавлениеFigure 1.3
CO: A 32‐year‐old woman presented with a soft hemorrhagic lump on her lower left gingivae.
HPC: The lump appeared three months ago and became gradually bigger, covering the whole crown of the second premolar, thus causing eating difficulties and phobias to the patient of being a malignant neoplasm.
PMH: A healthy woman at the third month after baby delivery, with no serious medical problems and drug use apart from iron and calcium tablets prescribed by her gynecologist during her pregnancy. Smoking or drinking habits were plentiful.
OE: A very soft penduculated mass on the gingivae from the distal part of the 1st lower right premolar to the 1st molar. It was very soft, vascular and sensitive, and was bleeding easily with slight probing and caused eating problems (Figure 1.3). The lesion developed gradually and reaching its biggest site at the last month of pregnancy and began to decrease slowly within the next three months after her delivery. No other similar lesions were found within her mouth, other mucosae or skin. Regional or systemic lymphadenopathy was not recorded.
Q1What is this lesion?
1 Kaposi's sarcoma
2 Pregnancy epulis
3 Peripheral giant cell granuloma
4 Gingival hemangioma
5 Peripheral ossifying fibroma
Answers:
1 No
2 Pregnancy epulis is a localized hyperplastic hemorrhagic soft lesion on the upper and lower gingivae of pregnant women with decayed teeth and poor oral hygiene. The lesion grows slowly and reaches its largest size during the last trimester of pregnancy.
3 No
4 No
5 No
Comments: In contrary to pregnancy epulis the gingival hemangiomas are found earlier (at childhood); sarcoma Kaposi are usually associated with lymphadenopathy and have an aggressive course. The peripheral odontogenic fibroma has a firmer feel on palpation, while the peripheral giant cell epulis does not improve with the baby's birth and is associated with endocrinopathies.
Q2Which are the other oral conditions seen during pregnancy?
1 Melasma
2 Pregnancy gingivitis
3 Increased risk of caries
4 Erosions of teeth
5 Sialorrhea
Answers:
1 No
2 Pregnancy gingivitis is the commonest complication of pregnancy and can start even from the second month, reaching its peak on the eight month of pregnancy. This type of gingivitis is due rather to the action of increased female hormones on their gingival receptors rather than to microbial plaque.
3 Pregnant women tend to be at increased risk of caries as the number of cariogenic bacteria in the mouth, and the frequency of eating, especially sweet food as a means of coping with nausea, are increased.
4 Erosions on the palatal tooth surface and especially on the upper anterior teeth are common and are also attributed to the acidity of gastric juice that reaches the mouth during vomiting.
5 Sialorrhea is a common finding in pregnant women and caused by the increased nausea and vomiting recorded during their pregnancy.
Comments: Melasma or pregnancy mask as it is known, is characterized by a brown discoloration of the facial skin and lips, but is never seen within the mouth of pregnant women and those taking contraceptives or hormone replacement medications.
Q3 Which conditions have been detected in babies, related to the periodontal status of their mothers?
1 Premature birth
2 Low weight
3 Vision or hearing deficits
4 Mental retardation
5 Dental anomalies
Answers:
1 Women with chronic inflammation of their gingivae seem to produce a number of inflammatory cytokines, some of which are responsible for the uterine muscle contractions which finally induce early labor.
2 Premature babies show incomplete growth and low weight.
3 Vision or hearing deficits are commonly seen in premature babies whose early birth may be associated with the periodontal problems of their mother.
4 No
5 No
Comments: The mental status of pregnant women may worsen their periodontal problems by increased secretion of cortisol and refusal of tooth brushing, while the periodontitis per se does not affect the mental status or dentition of their children.