Читать книгу Clinical Guide to Oral Diseases - Crispian Scully - Страница 18
Case 1.4
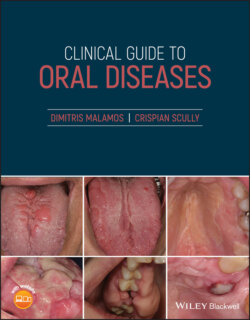
ОглавлениеFigure 1.4
CO: A 42‐year‐old woman came in with a hemorrhagic bulla inside her cheek.
HPC: The bulla appeared three hours ago after eating a sandwich. No similar bullae were recorded in her or her close relatives in the past.
PMH: From her medical records a few episodes of allergic rhinitis controlled with antihistamine and steroids in crisis were recorded. No blood and other systemic diseases, other allergies or drug uptakes were recorded.
OE: Examination revealed a large bulla with hemorrhagic content on the left buccal mucosa at the occlusion level (Figure 1.4). The bulla appeared during mastication and was easily broken during the examination's manipulations, leaving a painful superficial ulceration. No other bullae, ulcerations or petechiae and ecchymoses were seen on the oral and other mucosae or skin. Cervical lymphadenopathy was not seen.
Q1 Which is the disease responsible for this bulla?
1 Thrombocytopenia
2 Burns
3 Mucous membrane pemphigoid
4 Angina bullosa hemorrhagica
5 Hemorrhagic mucocele
Answers:
1 No
2 No
3 No
4 Angina bullosa hemorrhagica (ABH) is an acute, benign condition characterized by the development of subepithelial bullae filled with blood that are not attributed to any systemic disorders. A chronic trauma, consumption of hot and spicy or abrasive foods, or difficulties in restorative or periodontal treatment are considered to be the commonest causes.
5 No
Comments: Hemorrhagic bullae are often seen in other conditions such as thrombocytopenia, mucous pemphigoids and burns, but the presence of specific elements indicated the diagnosis. The appearance of low platelets and ecchymoses, epistaxis, and gingival bleeding in thrombocytopenia, the presence of numerous bullae with clear fluid in mucous pemphigoid, and the lack of close contact with thermal, chemical, or electrical elements in burns help to exclude these conditions from the diagnosis. Mucoceles are thicker and more resistant, while the bullae in angina are thinner and more easily break.
Q2 Which of the drugs below are usually related to the development of this condition?
1 NSAIDs
2 Antibiotics
3 Steroids
4 Anti‐diabetics
5 Bronchodilators
Answers:
1 No
2 No
3 Chronic use of steroids, especially inhalers, causes oral mucosa atrophy and decreases the submucosa's elastic fiber content, resulting in capillary breakdown locally, finally forming the characteristic hemorrhagic bullae.
4 No
5 No
Comments: Diabetes mellitus has also been associated with hemorrhagic bulla formation due to increased vascular fragility in these patients, and not to the drug for blood sugar reduction. Similar bullae could also be seen in patients who take antibiotics or bronchodilators and have various autoimmune diseases. As for NSAIDs, these drugs are responsible for peptic ulcers and bleeding from the intestine, but more rarely for skin bullous rash and fever.
Q3 Which of the histopathological finding(s) is/or are characteristics of this condition?
1 Subepithelial bulla
2 Intra‐epithelial abscess of neutrophils
3 Mononuclear inflammatory infiltration of submucosa deep to the muscles
4 Direct immunofluorescence negative
5 Eosinophils accumulation in the corium
Answers:
1 The breakage of the epithelial–connective tissue junction due to topical agents leads to local capillary hemorrhage and subepithelial bulla formation.
2 No
3 No
4 Direct immune‐fluorescence is always negative. DI is always positivein pemphigus and other intra‐epithelial blistering diseases.
5 No
Comments: The inflammatory response in ABH is intense and located only at the superficial parts of submucosa, often containing neutrophils but not eosinophils and mast cells.