Читать книгу Clinical Guide to Oral Diseases - Crispian Scully - Страница 22
Case 1.8
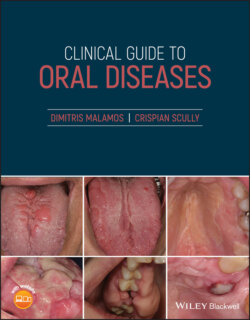
ОглавлениеFigure 1.8
CO: A 68‐year‐old woman was presented with hemorrhagic gingivae over the last three months.
HPC: Her gingivae showed areas of hemorrhage over the last three months and was associated with generalized lymphadenopathy, fever, weight loss and sweating at night.
PMH: Hyperlipidemia and diabetes mellitus were the only serious diseases reported. A recent blood check‐up revealed an increased number of eosinophils and lymphocytes as well as chronic sideropenic anemia, despite her proper diet. No smoking or drinking habits, but a chronic exposure to chemicals because of her job at a painting industry was reported.
OE: The examination revealed swollen, soft, edematous and hemorrhagic gingivae that were associated with a few scattered petechiae on buccal mucosae. The gingivae were pale and easily bled from the interdental papillae (Figure 1.8). A few ecchymoses were also found on her legs and associated with a generalized lymph node enlargement.
Q1 What is the cause of her gingival bleeding?
1 Acute ulcerative gingivitis
2 Scurvy
3 Leukemia
4 Plasma cell gingivitis
5 Wegener disease
Answers:
1 No
2 No
3 Leukemia is the cause. Leukemia is a malignant neoplasm of white blood cells characterized by an abnormal growth of a certain type of white cells, anemia, easy bruising or bleeding, susceptibility to infections, swollen lymph nodes, together with weight loss and night sweating, as was also observed in this patient who was finally diagnosed of having chronic lymphocytic leukemia
4 No
5 No
Comments: Gingival bleeding is a common finding in other local conditions such as in acute ulcerative and plasma cell gingivitis, or systemic diseases such as Wegener disease and scurvy. The lack of necrosis of interdental papillae (seen in acute ulcerative gingivitis) and the erythematous and edematous red attached gingivae (in plasma cell gingivitis) or the erythematous swollen‐like‐strawberries gingivae (in Wegener disease) and the ulcerated, swollen gingivae with deep pocketing (in scurvy) exclude the above diseases from the diagnosis.
Q2 Which laboratory tests are routinely used for the diagnosis of this condition?
1 White blood count
2 Immunophenotypic analysis with flow cytometry
3 Bone marrow biopsy
4 Urine analysis
5 Cerebral fluid biochemical analysis
Answers:
1 White blood count shows an increased number of lymphocytes (>10,000 cells/mm3).
2 The flow cytometric analysis of the bone marrow aspiration cells and peripheral blood cells with the use of a series of monoclonal antibodies allow the identification of hematologic malignancies including chronic lymphocytic leukemia (CLL).
3 Bone marrow biopsy is used in undiagnosed cases of blood dyscrasias showing the replacement of bone marrow cells with pathologic lymphocytes.
4 No
5 No
Comments: Urinalysis and cerebrospinal fluid (CSF) analysis are useful only in a diagnosis of aggressive leukemias like CLL, involving bladder and brain respectively.
Q3 Which other conditions are associated with this disease?
1 AnemiaThrombocytopeniaEosinophiliaComplement deficiencyParaproteinemiaAnswers:Anemia is a very common complication of CLL due to: (i) bone marrow accumulation of abnormal lymphocytes inducing the replacement of stem cells producing red cells; (ii) increased production of tumor necrosis factor (TNF) that suppresses red blood cell production; (iii) increased red cell destruction by circulated auto‐antibodies; and (iv) medications used for treatment of CLL that suppress red cell production.Thrombocytopenia is responsible for the increased bleeding tendency among patients with CLL.Eosinophilia is sometimes a preclinical sign of various hematological malignancies including lymphomas and CLL.Complement deficiency is a common finding and seems to limit CD20 monoclonal cytotoxicity in treatment’s efficacy for these patients.Monoclonal proteins are present in significant number of patients with CLL.