Читать книгу Clinical Guide to Oral Diseases - Crispian Scully - Страница 24
Case 1.10
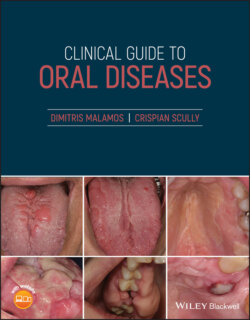
ОглавлениеFigure 1.10
CO: A 42‐year‐old man was admitted with gingival bleeding since the previous night.
HPC: The bleeding started suddenly after eating a snack with potato chips and became more intense and constant on the lower molar gingivae. No similar bleeding episodes had been reported previously by him or his close relatives.
PMH: Mild hypertension and cardiological problems were reported and controlled with diet and a heart mitral valve replacement five years ago, which was followed by daily use of the drug warfarin since then. Allergies or other systemic diseases and smoking or drinking habits were not recorded, while his diet was poor in green vegetables only.
OE: Spontaneous bleeding from all his gingivae but mainly from his lower left molars with incomplete clot formation was noticed. The clot was very soft and there was constant bleeding arising from the interdental papillae (Figure 1.10). This did not end with pressure, rinses with cold saline mouthwashes or antiseptics. A few petechiae were also seen near the occlusal lines of the buccal mucosae, but also in other mucosae or the skin. Cervical or systemic lymphadenopathy was also missing.
Q1 What is the main cause of gingival bleeding?
1 Local trauma
2 Dental plaque
3 Warfarin‐induced
4 Vitamin C deficiency
5 Liver cirrhosis
Answers:
1 Local trauma induced from hard foods such as potato chips could be a predisposing factor for gingival bleeding in patients regardless their oral hygiene status.
2 No
3 Warfarin is the main cause, as it blocks one of the enzymes that use vitamin K to produce clotting factors, thus causing incomplete clot formation similar to that was seen in this patient.
4 No
5 No
Comments: Dental plaque is responsible for gingival infection and bleeding in healthy and diseased patients, but it does not affect the clotting cascade. A vitamin C deficiency can cause alterations in collagen synthesis, making the small vessels of the gingivae weak and vulnerable to easy bleeding, either with a minor trauma or automatically. However, the patient's diet is correct, without any alcohol use and includes a great a number of foods that are rich in Vitamin C, apart from green fruits and vegetables which were excluded due to his warfarin uptake.
Q2 Which is/are the blood test/s used for checking a bleeding disorder?
1 WBC
2 D‐dimers
3 PT
4 A PTT
5 Vitamin D levels
Answers:
1 White blood count (WBC) is required to check the number of platelets (thrombocytopenia) as well as the presence of anemia.
2 D‐dimers measure a specific type of cross‐linked fibrin degradation, while the elevated levels are indicators of recent clotting activity such as clotting dissemination or intravascular coagulation.
3 Prothrombin time (PT) is the time for blood to clot in a general screen that evaluates factors VII, X, II and II.
4 Activated partial thromboplastin time, also known as A PTT, is a sensitive indicator of coagulation and evaluates additionally to PT factors such as prekallikrein, factors VII, IX and high molecular weight kininogen, and examines how both the intrinsic clotting pathway and the common final pathway are working.
5 No
Comments: Vitamin D is required for regulation of calcium and phosphorus in the body. Its deficiency is common and related to osteoporosis in older patients and rickets in children but not with clotting diseases.
Q3 Which of the drugs below enhance the bleeding?
1 Aspirin
2 Fluconazole
3 Metronidazole
4 Phenytoin
5 Omeprazole
Answers:
1 Aspirin is often used together with warfarin in patients with valve replacement and increases the bleeding tendency, but it is always dependent on the intensity of the treatment.
2 Fluconazole is the drug of choice for various fungal infections. In combination with warfarin, it can increase the hypoprothrombinemic effect of the second drug by interfering with its metabolism and inhibiting the liver enzymes CYP450 2C19 and 3A4.
3 Metronidazole increases the plasma concentration of warfarin by inhibiting the action of CYP450 2CR enzyme that is responsible for the metabolic clearance of the active enantiomers of warfarin.
4 No
5 Omeprazole is sometimes related to an increased action of warfarin, but their interaction seems to have a minor, doubtful or limited clinical significance.
Comments: Phenytoin, a well‐known antiepileptic drug, has a complex interaction with warfarin. It initially increases but later reduces INR after a prolonged application.