Читать книгу Clinical Guide to Oral Diseases - Crispian Scully - Страница 33
Case 2.8
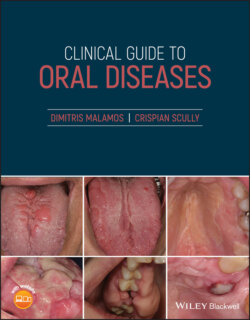
ОглавлениеFigure 2.8
CO: A 52‐year‐old woman was admitted with one week history of bluish discoloration of her tongue.
HPC: Half of her tongue was swollen, sensitive on touching with a bluish discoloration which appeared after an episode of collapse one week ago.
PMC: She had no serious medical problems apart from low blood pressure which sometimes caused her dizziness and instability. She suffered from iron deficiency anemia, in the past, which was resolved as the patient entered the menopause. No other blood diseases or bleeding dyscrasias were reported. She is a non‐smoker or drinker and has never chewed her lips or tongue.
OE: The oral examination revealed a diffuse swelling on the right part of her tongue that was associated with a small healing ulcer, yellow coat of debris and necrotic papillae. The swelling is painful on palpation and has a bluish discoloration extended to the lateral margin of her tongue (Figure 2.8). No other similar lesions, petechiae or ecchymoses were seen within the oral mucosa or other mucosae and skin nor evidence of bleeding in internal organs like liver, kidney or even brain.
Q1 What is the main cause of this blue discoloration?
1 Enlarged tongue vessels
2 Hemangioma
3 Hemosiderosis
4 Traumatic hematoma
5 Lymphangioma
Answers:
1 No
2 No
3 No
4 After a collapse, tongue biting commonly happens and can cause swelling and hematoma formation locally. The hematoma was formed by seeping and accumulation of blood within the tongue submucosa from broken capillaries due to trauma causing a bluish discoloration of this area.
5 No
Comments: Superficial vascular tongue lesions like hemangiomas and lymphangiomas or enlarged vessels cause often a bluish discoloration but are excluded as these malformations of the lymphatic system (lymphangiomas) or blood vessels (hemaniomas) are usually presented at a very early age (birth or infancy) and are unrelated to any local trauma. Hemosiderosis should also be ruled out from the diagnosis as the patient's medical history is negative for severe anemias or diseases requiring blood transfusion or drugs rich in iron, and this condition appears in many parts of the body apart from the mouth.
Q2 The necessity for urgent treatment of hematoma is mainly dependent on:
1 Location
2 Color
3 Syptomatology
4 Size
5 Patient's age
Answers:
1 Hematomas may occur anywhere in the body, but skull hematomas are the most dangerous and require immediate treatment, as they can increase intracranial pressure and seriously impair various brain functions.
2 No
3 Symptomatology of hematoma (swelling or pain) is sometimes very alarming and patients must seek immediate surgical (drainage) or clotting treatment (altering or stopping the responsible medicines).
4 Large hematomas have a higher risk of altering basic functions of the tissues involved such as the brain and other vital organs, and require immediate treatment.
5 No
Comments: Hematomas appear initially as dark blue or black lesions whose color is dependent on the amount of accumulated blood or its location's depth and duration, but is not associated with prognosis. Hematomas that are resolved within one to two weeks despite the patient's age, change their color from dark blue to yellow, and do not pose a risk to the patient's life.
Q3 Which investigations are required for the diagnosis of a traumatic‐induced skull hematoma?
1 Neurological tests
2 Cerebrospinal fluid analysis
3 Skull CT/MRI
4 Clotting blood tests
5 Respiratory tests
Answers:
1 Neurological tests should be undertaken to examine the degree of consciousness, ataxia, or nystagmus as well as the sensory or motor deficits which might have been provoked by a subdural hematoma.
2 Analysis of the cerebrospinal fluid in patients with traumatic intracranial hematoma reveals an increased level of glucose, lactate, and lactate dehydrogenase (LDH) as well as a predominance of monocytes or polymorphonuclear cells at the cellular level.
3 CT or MRI of the skull shows the location and severity of skull hematoma and its response to treatment.
4 No
5 No
Comments: Clotting tests are useful for the detection of hemostasis dysfunctions rather than trauma‐induced intracranial hemorrhage, while the respiratory tests are only required when the hematoma is severe and might affect the respiratory centers in the pons and medulla oblongata in the brainstem.