Читать книгу Clinical Guide to Oral Diseases - Crispian Scully - Страница 38
Case 3.2
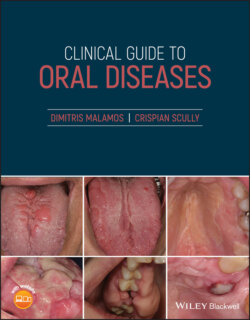
ОглавлениеFigure 3.2a
Figure 3.2b
CO: A 72‐year‐old woman was referred for evaluation of multiple brown lesions in her mouth.
PMH: She suffered from polycythemia vera which was diagnosed 15 years ago. It was controlled with hydroxyurea tablets. A small hormone‐sensitive carcinoma in situ of her right breast was removed; letrozole tablets are now her maintenance treatment. She has never been hypotensive or allergic to various drugs or foods, nor a smoker or drinker.
HPC: The brown lesions in her mouth were accidentally found during a clinical examination by her physician two weeks ago.
OE: During the examination, multiple brown lesions scattered on the dorsum and lateral margins of the tongue (Figure 3.2a), buccal mucosae and soft palate and were linked with skin pigmentation and brown discoloration of the nail hands and feet (melanonychia) (Figure 3.2b). No other abnormalities either on the skin or other organs were reported, and her blood tests, including various hormone tests, were in a normal range.
Q1 What is the cause of her oral and skin pigmentation?
1 Addison's disease
2 Melanoma, widespread
3 Chemical poisoning
4 Drug‐induced pigmentation
5 Cushing's disease
Answers:
1 No
2 No
3 No
4 The use of hydroxyurea and not letrozole has been associated with the increased pigmentation in this patient. Hydroxyurea is routinely used as an anti‐neoplastic agent for the treatment of various myeloproliferative disorders such as leukemias, thrombopenias, polycythemia, and sometimes in psoriasis. Hydroxyurea can cause increased melanin production thus showing dark brown pigmentation of skin, sclera, nails of hands and feet and oral mucosa within a few months of treatment.
5 No
Comments: The normal blood pressure together with the normal hormone levels and the clinical characteristics and slow pigmentation progress exclude Cushing's, Addison's diseases and melanoma from the diagnosis.
Q2 What other drugs can cause hyper‐pigmentation?
1 Anti‐malarials
2 NSAIDs
3 Antibiotics
4 Cytotoxic drugs
5 Anti‐emetics
Answers:
1 Anti‐malarials such as chloroquine or hydroxychloroquine, having been used for months, can cause blue or gray pigmentation on face, neck, legs, and nails.
2 NSAIDs are used for pain or inflammation relief and sometimes cause a fixed drug reaction which initially appears in the form of erythematous lesions on the face, lower extremities or genitalia, leaving, eventually, a brown discoloration.
3 Antibiotics and especially tetracyclines cause brown discoloration of nails, sclera, skin, and bones.
4 Cytotoxic drugs cause a brown discoloration as a transverse or longitudinal band of the nail bed and other mucosae which gradually fades with drug withdrawal.
5 No
Comments; Anti‐emetic drugs are widely used against nausea and vomiting in motion sickness, gastroenteritis and during chemotherapy, and are mostly related to dry mouth, constipation, fatigue, and drowsiness rather than skin discoloration.
Q3 Which drug mechanism induces pigmentation?
1 Activation of melanocytes for melanin production
2 Inhibition of melanophage action
3 Deposition of drug into the tissues
4 Extravagation and disintegration of red blood cells from the small vessels in the lamina propria
5 Vasodilatation due to drug‐induced inflammation
Answers:
1 Various drugs increase the production of melanin from active melanocytes within the basal layer.
2 No
3 Deposition of the causative drug or its complex with melanin can cause discoloration of the tissues.
4 No
5 No
Comments: Certain drugs could trigger local inflammation causing vasodilation and in some places hemorrhage, and breakdown of hemoglobulin of the red blood cells, with final production of hemosiderin. This is an iron storage complex whose excessive accumulation into various tissues, known as hemosiderosis, causes secondary black to brown discoloration. The presence and the number rather than the action of melanophages seems to play a role in inflammatory pigmented skin lesions.