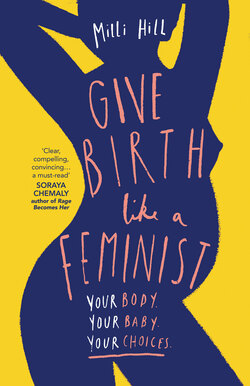
Читать книгу Give Birth Like a Feminist - Милли Хилл - Страница 7
The Language of Permission
ОглавлениеIn the months and years that followed I began to listen to other women’s birth stories with a keen ear, waiting to hear for the tipping point where they had either triumphed or, as I had, slipped beneath the waves. In every story from across the Western world I heard the same words over and over: ‘They did not let me’, and ‘I was not allowed’. I heard it so much so that I gave this phenomenon its own special name, ‘The Language of Permission’.
‘I had to have a vaginal exam, as soon as I arrived at the hospital, to check if I was in labour.’
‘I wanted to have a water birth, but I was not allowed to use the birth centre[fn1] because of my BMI, so I had to be on labour ward.’
‘Because I was trying for a VBAC,[fn2] I was not allowed to eat or drink in labour, in case I ended up having another caesarean.’
‘My partner wanted to come with me for that part, but he was not allowed.’
‘They don’t let you have skin to skin with your baby after a caesarean in my hospital.’
‘They told me not to push yet even though I was desperate to.’
… and so it went on.
I began to wonder how these phrases were tripping so readily off our tongues as women of the twenty-first century. We would not accept being restricted in this way in our relationships or marriages, in our educational choices, or in our career paths. Why, when it came to giving birth – arguably a pretty significant moment in a woman’s life – were we using such passive language, casting ourselves as the ‘permission seekers’, rather than the ‘permission givers’?
The answer to why we have this imbalance of power, I’ve discovered, is complex, and emotional, but, if you put it in a big pot and simmer it for a long time, it boils down to a few interconnected essentials:
Fear of birth is at an all-time high
Confusion over the rights of the fetus can cause ‘risk’ to trump ‘autonomy’
And finally, we live in a patriarchy.
Let’s start with the fear. In the twenty-first-century birth room, everyone – women, partners, midwives and doctors alike – is, either consciously or unconsciously, terrified of birth. This fear, which a hundred years ago may have taken the form of low-level anxiety or healthy respect, has transmogrified in recent decades into full-scale panic. Where birth was once a large stray dog that you generally expect to be friendly but approach with caution, it now seems to have evolved into a many-headed monster-hound, rumoured to be loose on the moor, with occasional sightings reported in hushed tones. Like death, birth has become something we’ve lost touch with, that no longer takes place in our communities and that we therefore rarely see or hear. Women go to the hospital and come back with a baby, and what happens in the intervening day or two remains a somewhat terrifying mystery. If we do see birth, it’s quite likely to be a representation on TV, which, as we’ll explore in Chapter 6, may be a long way from accurate.
In all areas of life, fear can make prisoners of us, and birth is no different. Our fear may shape our behaviour, our expectations, and, in turn, our actual reality. In fear, we may not prepare for birth, believing it to be ‘unpredictable’, or we may decline to ask questions, feeling that we are powerless. In modern maternity care, medical professionals and parents-to-be alike are often found erring on the side of caution, and this defensive behaviour can be at the expense of personal freedom. Which brings us to the overlapping concern of point two, the safety of the unborn child, another key player in the birth room power imbalance. Modern maternity care is rightly focused on birth outcomes, but a good outcome is most often measured not in terms of the woman, her feelings, her experience, and her postnatal mental health, but on the idea of the ‘healthy baby’ – indeed, women are frequently told that this is all that matters.
Of course, for most of us, the welfare of our baby is the most important aspect of the birth experience, but it’s interesting how this idea that it is all that matters has really started to trip off the tongue in the last few decades. It has become a mantra, and hidden beneath it is a rather dark, unspoken message: women do not matter. In a power dynamic in which you are given the message – however subtle – that your needs and feelings are of secondary importance, it can be difficult to challenge those who are perceived to be in authority, or even to voice your discomfort. New mothers who have had what feminist Naomi Wolf calls ‘ordinary bad births’ – or even suffered severe trauma – are told repeatedly to ‘focus on their healthy baby’, as this is ‘what really matters’, and while this may be well-meant reassurance, to many it carries the subtext, ‘Be quiet about your bad birth now please’, or, worse still, ‘Aren’t you grateful for your baby – don’t you love them?’
There is also an assumption that ‘safety’ and ‘health’ begin and end with simply having a pulse. However, as many women who have had what may look from the outside like fairly straightforward births will reiterate, feeling that you are safe can be very subjective, and being healthy is more complicated that simply looking OK on the surface. Feelings of trauma, sadness, shame, guilt, powerlessness, violation, and regret pervade the postnatal experience and reach far into the future mental and emotional well-being of women, and by default their relationships not just with themselves, but with their partners and children too. Statistics vary, but traumatic birth in the UK alone is estimated to affect nearly one in three women a year,[2] with many of those – between 4 per cent and 18 per cent – going on to develop PTSD.[3] Still others may not necessarily raise their hand to feeling full-blown trauma, but, if you ask them about their birth story, will tell you of a catalogue of missed opportunities to treat them with kindness, respect or tenderness, and sometimes atrocious treatment that they would never have felt they had the right to complain about.
During pregnancy itself, women are also reminded that the pinnacle of their birth expectations should be a healthy baby, most often at times when they show signs of having done their research and thus being keen to take an active role in the decision making. ‘Birth plans’ are a crucible for this phenomenon – a woman who goes so far as to outline on paper what she would like to happen to her in labour will be discouraged, at best, or even openly mocked, as we saw in November 2017 when a group of doctors caused outrage on Twitter when they joked that, ‘the length of the birth plan directly correlates to the length of the caesarean incision’, and that laminated birth plans were only useful if the woman had a massive haemorrhage.